TME Combination Therapy Selector
Select Dominant TME Cell Type
Myeloid-Derived Suppressor Cells (MDSC)
Primary suppressive cells in CLL and MCL that inhibit T-cell activity
Tumor-Associated Macrophages (TAM)
M2 phenotype dominates in many B-cell malignancies, promoting tumor growth
Regulatory T Cells (Treg)
Modulates immune response and suppresses anti-tumor immunity
B-Cell Receptor Signaling
Primary pathway targeted by ibrutinib in malignant B cells
Recommended Combination
Select a dominant TME cell type to see optimal combination therapy
Note: Combination therapies require careful monitoring of side effects
When doctors first started using ibrutinib for B‑cell cancers, they noticed something unexpected: the drug seemed to reshape the whole neighborhood around the tumor, not just kill the cancer cells directly. Understanding how ibrutinib interacts with the tumor microenvironment (TME) helps explain its lasting responses and points to new combo strategies.
Key Takeaways
- Ibrutinib blocks BTK, which dampens pro‑survival signals in malignant B cells.
- Beyond cancer cells, ibrutinib modulates immune cells in the TME, reducing suppressive myeloid cells and altering cytokine gradients.
- Clinical trials show improved progression‑free survival in CLL and MCL when ibrutinib is paired with checkpoint inhibitors.
- Side‑effects such as bleeding or atrial fibrillation arise from off‑target inhibition of Tec family kinases.
- Future research focuses on fine‑tuning dosing schedules to maximize immune re‑education while minimizing toxicity.
What Is Ibrutinib?
Ibrutinib is a covalent Bruton tyrosine kinase (BTK) inhibitor approved for several B‑cell malignancies, including chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL). Developed by Pharmacyclics and FDA‑approved in 2013, the drug binds irreversibly to the C481 residue of BTK, shutting down B‑cell receptor (BCR) signaling and inducing apoptosis.
How Ibrutinib Targets BTK
Bruton tyrosine kinase (BTK) is a key enzyme in the BCR pathway. When BTK is active, it triggers downstream NF‑κB and MAPK cascades that promote proliferation and survival of malignant B cells. Ibrutinib’s covalent attachment prevents ATP binding, halting these cascades. Because BTK is also expressed in several innate immune cells, the drug’s reach extends into the TME.
The Tumor Microenvironment Explained
Tumor microenvironment (TME) comprises cancer cells, stromal fibroblasts, vascular networks, extracellular matrix, and a host of immune cells like myeloid‑derived suppressor cells (MDSC), tumor‑associated macrophages (TAM), and regulatory T cells (Treg). These components create a niche that can either support or hinder tumor growth.
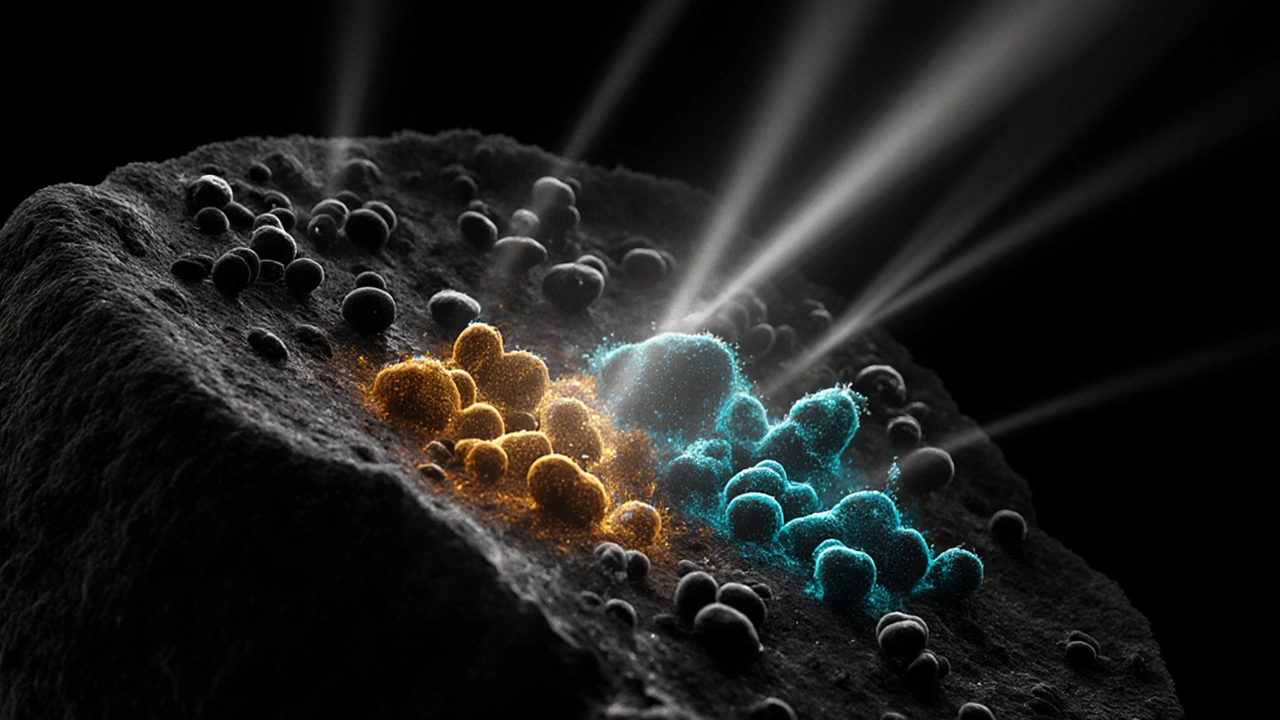
Direct Effects of Ibrutinib on Immune Cells
While the primary target is BTK in B cells, ibrutinib also hits BTK‑expressing myeloid cells. The most notable changes include:
- Myeloid‑derived suppressor cells - reduced frequency and impaired suppressive function, leading to enhanced T‑cell activation.
- Tumor‑associated macrophages - shift from an M2‑like (pro‑tumor) phenotype toward an M1‑like (anti‑tumor) profile, marked by increased IL‑12 and decreased IL‑10 production.
- Regulatory T cells - modest decline in FoxP3⁺ cells within the lymph node, relieving local immunosuppression.
These alterations are largely BTK‑dependent but also involve off‑target inhibition of Tec and SRC family kinases, which affect cytokine signaling.
Indirect Effects: Cytokine and Chemokine Remodeling
Ibrutinib reshapes the cytokine milieu. Studies in CLL patients reported lower serum levels of IL‑6, CXCL12, and CCL3 after six months of therapy. Reduced CXCL12 gradients impair the homing of malignant B cells to protective bone‑marrow niches, making them more vulnerable to immune clearance.
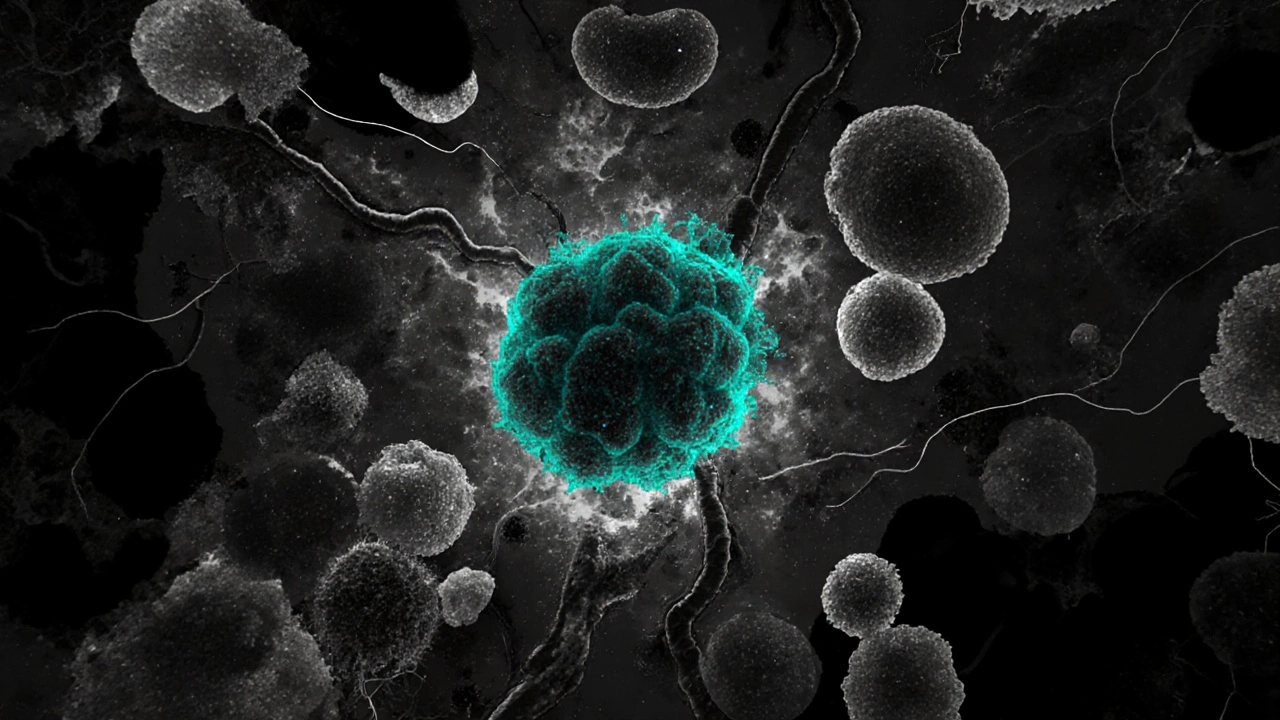
Clinical Evidence of TME Modulation
Several trials have quantified these immune shifts:
- In a phaseII CLL study (n=60), flow cytometry showed a 45% drop in circulating MDSC counts after 12weeks of ibrutinib.
- A multicenter MCL trial combined ibrutinib with anti‑PD‑1 therapy; the overall response rate rose from 68% (ibrutinib alone) to 84%, correlating with increased CD8⁺ T‑cell infiltration in tumor biopsies.
- Long‑term follow‑up of CLL patients (median 5years) revealed that patients with early TAM phenotype conversion had longer progression‑free survival.
These data suggest that the drug’s benefit extends beyond direct cytotoxicity.
Combination Strategies Leveraging TME Effects
Because ibrutinib opens the immune gate, researchers are trialing combos that further stimulate anti‑tumor immunity:
- Checkpoint inhibitors (anti‑PD‑1, anti‑CTLA‑4) - aim to capitalize on increased CD8⁺ activity. \n
- PI3Kδ inhibitors - synergize by blocking parallel survival pathways.
- CAR‑T cell therapy - pre‑treatment with ibrutinib can reduce exhaustion markers on infused T cells.
Choosing the right partner depends on the dominant suppressive cell type in a given cancer. For example, if MDSC enrichment is the main barrier, adding a CSF‑1R inhibitor may be most effective.
Practical Considerations & Safety Profile
While reshaping the TME is attractive, clinicians must balance benefits with adverse events. Off‑target inhibition can cause:
- Bleeding tendencies (platelet aggregation impairment).
- Atrial fibrillation (likely due to Tec kinase inhibition in cardiac tissue).
- Infections - especially opportunistic fungal infections when immune re‑education is profound.
Monitoring guidelines recommend baseline ECG, periodic CBC, and vigilance for bruising. Dose adjustments (420mg vs. 560mg) can mitigate some risks without losing TME modulation.
Future Directions
Next‑generation BTK inhibitors (e.g., acalabrutinib, zanubrutinib) aim for higher selectivity, hoping to preserve immune‑modulating benefits while reducing cardiac toxicity. Meanwhile, spatial transcriptomics is being used to map how ibrutinib reshapes the TME at a single‑cell level, guiding personalized combo regimens.
Frequently Asked Questions
How does ibrutinib differ from traditional chemotherapy?
Chemotherapy kills rapidly dividing cells indiscriminately, while ibrutinib specifically blocks BTK signaling. This targeted approach not only halts cancer‑cell growth but also re‑programs immune cells in the tumor microenvironment, leading to a more durable response.
Can ibrutinib be used for solid tumors?
Direct approvals are limited to B‑cell malignancies. However, early-phase trials are testing ibrutinib in combination with immunotherapy for pancreatic and breast cancers, exploiting its ability to reduce myeloid suppression.
What is the typical dosing schedule?
The standard oral dose is 420mg once daily for CLL and 560mg for MCL, taken with water. Some clinicians lower the dose to 280mg if patients develop atrial fibrillation or significant bleeding.
How quickly does the tumor microenvironment change after starting treatment?
Peripheral blood analyses show reductions in MDSC counts within 2-4weeks, while tissue biopsies often reveal macrophage phenotype shifts by 8-12weeks.
Are there biomarkers to predict who will benefit most?
High baseline BTK expression, low CXCR4 signaling, and pre‑existing CD8⁺ infiltration have been associated with better responses. Ongoing trials are validating composite scores that include these parameters.
Summary Table of Ibrutinib’s TME Impact
| Cell Type | Primary Effect | Clinical Relevance |
|---|---|---|
| Myeloid‑derived suppressor cells | Reduced frequency and suppressive activity | Enhanced CD8⁺ T‑cell response; predicts longer PFS |
| Tumor‑associated macrophages | Shift from M2 to M1 phenotype | Improved tumor clearance; synergy with checkpoint blockade |
| Regulatory T cells | Modest decrease in numbers | Relieves local immunosuppression, especially in CLL nodes |
| B‑cell malignancies (CLL, MCL) | Inhibition of BTK‑driven survival signaling | Direct tumor shrinkage; foundation of FDA approvals |
By looking at both the cancer cells and the surrounding ecosystem, clinicians can leverage ibrutinib’s dual action to design smarter, more durable treatment plans.
Louis Robert
October 15, 2025 AT 20:46Ibrutinib’s ability to re‑program the tumor microenvironment is a great example of targeted therapy acting beyond tumor cells. By dampening MDSC numbers and shifting macrophages toward an M1 phenotype, it creates a more immunogenic niche.
tim jeurissen
October 20, 2025 AT 11:53It is elementary to observe that the pharmacodynamic profile of ibrutinib extends to non‑malignant leukocytes, thereby effecting a systemic immunomodulation that is frequently under‑appreciated in conventional oncology discourse.
lorna Rickwood
October 25, 2025 AT 03:00One could argue that the drug does more than just kill cells it also reshapes the whole ecosystem around the tumour which in turn changes how the body reacts to the disease
Mayra Oto
October 29, 2025 AT 17:06From a global perspective the rollout of ibrutinib has highlighted differences in monitoring protocols across countries; the UK, for instance, emphasizes ECG checks before starting therapy.
S. Davidson
November 3, 2025 AT 08:13While the immunologic shift is appealing, clinicians must remember that the drug’s off‑target inhibition of Tec kinases is the root cause of atrial fibrillation, a risk that cannot be glossed over in enthusiasm.
Haley Porter
November 7, 2025 AT 23:20The mechanistic underpinnings of ibrutinib’s TME modulation involve intricate feedback loops between BTK‑dependent signaling cascades and cytokine networks. By attenuating CXCL12 gradients, malignant B‑cells lose their homing advantage, rendering them vulnerable to cytotoxic T‑lymphocytes. Simultaneously, the drug curtails STAT3 activation in myeloid‑derived suppressor cells, diminishing their suppressive capacity. This duality-direct tumouricidal activity coupled with immune re‑education-positions ibrutinib as a bridge between targeted therapy and immunotherapy.
Samantha Kolkowski
November 12, 2025 AT 14:26It’s interesting to see how the cytokine remodeling dovetails with checkpoint blockade; the increased CD8+ infiltration observed in combination trials suggests a synergistic potentiation.
Nick Ham
November 17, 2025 AT 05:33The side‑effects outweigh the marginal TME benefits.
Jennifer Grant
November 21, 2025 AT 20:40When we examine the longitudinal data from CLL cohorts, a pattern emerges that is both nuanced and instructive. First, the reduction in circulating MDSC counts is detectable within the first month of therapy, indicating a rapid pharmacodynamic response. Second, tissue biopsies reveal a phenotypic shift in tumor‑associated macrophages from an M2‑like to an M1‑like state by weeks eight to twelve, a timeline that aligns with the observed increase in intratumoral IL‑12 levels. Third, patients who exhibit an early decline in FoxP3+ regulatory T‑cells tend to enjoy longer progression‑free survival, suggesting that Treg modulation may be a predictive biomarker. Fourth, the off‑target inhibition of Tec kinases, while responsible for atrial fibrillation, also appears to blunt platelet aggregation, thereby complicating anticoagulation strategies in at‑risk populations.
Fifth, the interplay between BTK inhibition and the CXCR4/CXCL12 axis reduces marrow homing, effectively mobilizing malignant cells into peripheral blood where they become more susceptible to immune clearance. Sixth, combination approaches that pair ibrutinib with anti‑PD‑1 antibodies have demonstrated response rates climbing from the high‑sixties to the mid‑eighties, a testament to the drug’s role as an immune primer.
Seventh, emerging next‑generation BTK inhibitors such as acalabrutinib and zanubrutinib retain the TME‑modulating advantages while sparing cardiac tissue, offering a more favorable safety profile. Eighth, spatial transcriptomics studies are now mapping the microenvironmental re‑wiring at single‑cell resolution, revealing heterogeneity that may explain variable patient outcomes.
Ninth, the durability of response appears linked to the persistence of M1‑polarized macrophages, which continue to secrete pro‑inflammatory cytokines long after drug discontinuation. Tenth, future clinical trials are exploring triple‑combo regimens that incorporate BTK inhibition, checkpoint blockade, and CSF‑1R antagonism to target residual immunosuppressive myeloid populations.
Finally, while the data are promising, vigilant monitoring for bleeding, infections, and arrhythmias remains paramount. As we refine dosing schedules and patient selection criteria, the goal is to harness the full spectrum of ibrutinib’s immunologic effects without compromising safety.
Kenneth Mendez
November 26, 2025 AT 11:46All this talk of ‘immune re‑education’ is just a smokescreen. Big Pharma wants us to believe the side‑effects are manageable while they push a drug that subtly rewires our biology to make us dependent on perpetual prescriptions.
Gabe Crisp
December 1, 2025 AT 02:53The narrative that we’re being “re‑educated” is frightening; it suggests a loss of personal agency, and that’s exactly what those controlling the drug pipeline want-compliance through pharmacology.
Paul Bedrule
December 5, 2025 AT 18:00The ontological implications of modifying the tumor microenvironment extend beyond oncology, hinting at a broader philosophical shift in how we conceptualize disease and therapeutic agency.
yash Soni
December 10, 2025 AT 09:06Oh great, another “miracle” drug that pretends to fix everything while quietly stealing your wallet.
Emily Jozefowicz
December 15, 2025 AT 00:13Sure, if you enjoy paying premium prices for a pill that occasionally makes your immune system a little nicer to you, then by all means keep buying it.
Franklin Romanowski
December 19, 2025 AT 15:20Overall, the data suggest that when used thoughtfully and monitored closely, ibrutinib can provide a meaningful boost to anti‑tumor immunity while keeping side‑effects in check.