If you’ve been feeling constantly on edge, worrying about everything from your job to your health to what might happen tomorrow, you’re not alone. About 6.8 million adults in the U.S. live with Generalized Anxiety Disorder (GAD) each year. It’s not just stress. It’s a persistent, overwhelming sense of dread that doesn’t go away-even when there’s no clear reason for it. And if you’ve been told to take a pill or try therapy, you’re probably wondering: which one actually works? And is one safer than the other?
What Exactly Is Generalized Anxiety Disorder?
GAD isn’t just being a worrier. According to the DSM-5, it’s when you experience excessive worry on more days than not for at least six months. That worry is hard to control and comes with physical symptoms like muscle tension, trouble sleeping, fatigue, or difficulty concentrating. It’s not about being nervous before a presentation-it’s about being nervous about the presentation, then the meeting after, then whether you’ll get sick next week, then whether your car will break down, then whether your kids are safe… and so on. It’s exhausting. And it gets in the way of living.SSRIs: The Slow Burn That Lasts
Selective Serotonin Reuptake Inhibitors-SSRIs-are the most commonly prescribed medications for GAD today. Drugs like escitalopram (Lexapro), sertraline (Zoloft), and paroxetine (Paxil) work by increasing serotonin levels in the brain. But here’s the catch: they don’t work right away. It takes 2 to 6 weeks before you start feeling better. Some people don’t notice changes until week 8. Why do doctors still push them? Because they work-and they stick around. In clinical trials, about 50 to 60% of people with GAD see a meaningful drop in symptoms after 12 weeks. What’s more, when you stop taking them, the anxiety doesn’t come rushing back as hard as it does with other meds. That’s because SSRIs don’t just mask symptoms-they help rewire how your brain responds to stress over time. Side effects? Yes. Nausea, especially at first. Sexual dysfunction affects nearly half of users. Some feel jittery or sleepy. But these usually fade after a few weeks. Most people tolerate them well if they start low and go slow. Doctors often begin with half the usual dose-like 25mg of sertraline-and bump it up weekly to avoid the worst of the early side effects. And here’s something important: SSRIs help when anxiety comes with depression. About 60% of people with GAD also have depression. SSRIs treat both at once. Benzodiazepines? They don’t touch depression.Benzodiazepines: Fast Relief, Big Risks
If you’ve ever had a panic attack so bad you thought you were dying, you know why benzodiazepines like alprazolam (Xanax), lorazepam (Ativan), or diazepam (Valium) feel like a lifesaver. They kick in within 30 to 60 minutes. They calm your racing heart, quiet your mind, and make breathing easier. For acute moments-before a flight, during a crisis-they’re powerful. But here’s the problem: they don’t fix the root cause. They just put a bandage on it. And after a few weeks, your brain starts to adapt. You need more to get the same effect. That’s tolerance. And then, when you try to stop? Withdrawal can be worse than the original anxiety-shaking, insomnia, rebound panic, even seizures in extreme cases. Studies show that 40 to 50% of people on long-term benzodiazepines end up needing higher doses. The FDA now requires a black box warning on these drugs for abuse, dependence, and withdrawal. That’s the highest level of warning they give. They’re also risky if you drink alcohol, take opioids, or have a history of addiction. The CDC and NICE guidelines say they should never be first-line treatment. They’re for short-term use-2 to 4 weeks max-unless there’s no other option. Even then, doctors should monitor closely and taper slowly. The Ashton Manual, written by a leading expert, recommends taking 8 to 16 weeks to safely come off benzodiazepines.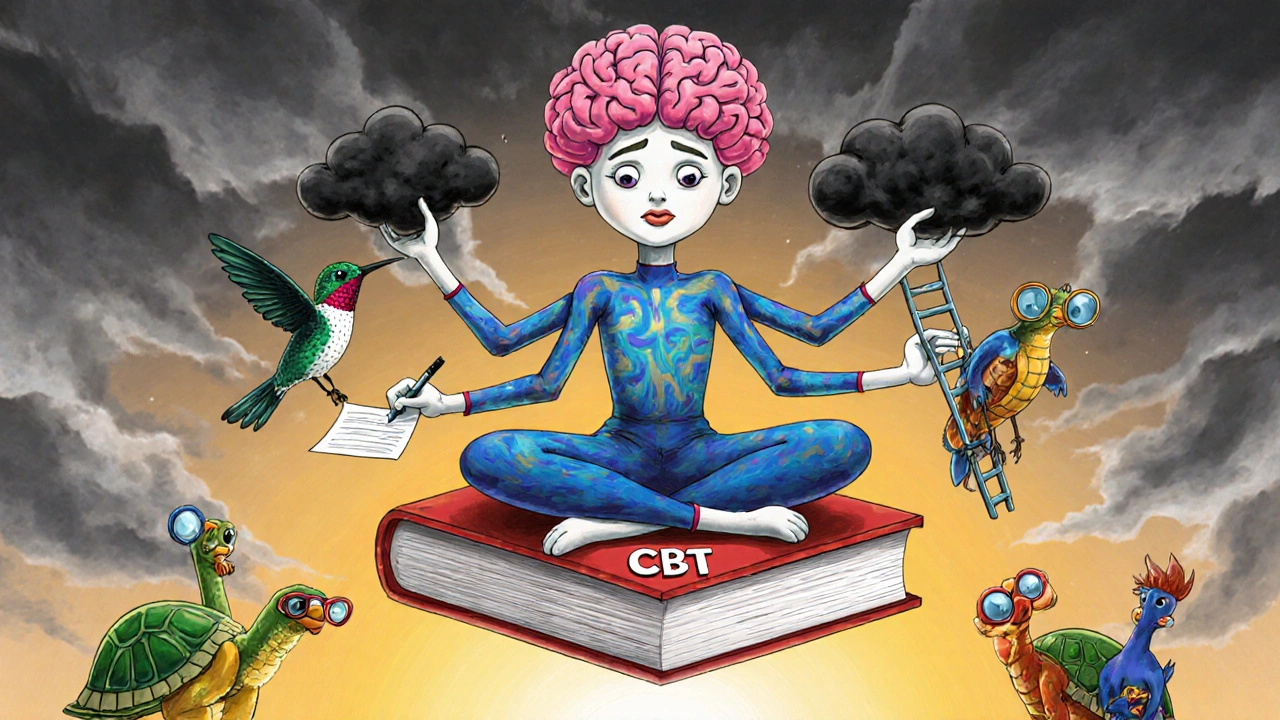
Cognitive Behavioral Therapy (CBT): Rewiring Your Thoughts
CBT is the only treatment here that doesn’t involve a pill. It’s a structured, time-limited therapy-usually 12 to 20 weekly sessions. You work with a therapist to identify the thoughts that fuel your anxiety. Maybe you think, “If I make a mistake at work, I’ll get fired and end up homeless.” CBT helps you test that thought. Is it true? What’s the evidence? What’s the worst that could realistically happen? You also learn exposure techniques. Instead of avoiding situations that scare you, you face them in small, controlled steps. If you’re afraid of social gatherings, you might start by saying hi to one person. Then two. Then staying for 10 minutes. Then 30. It’s uncomfortable at first-63% of patients say the exposure exercises are the hardest part-but that’s where the change happens. The results? Just as effective as SSRIs after 12 weeks. But here’s the kicker: after a year, people who did CBT are less likely to relapse. Only 25% return to high anxiety levels, compared to 45% who stopped taking medication. Why? Because CBT gives you tools. You don’t need the therapist forever-you keep the skills. The downside? Access. There are only about 0.5 certified CBT therapists per 10,000 adults with anxiety in the U.S. Sessions cost $100 to $150 each. Insurance covers some, but not always well. That’s why digital CBT apps like Woebot and SilverCloud are gaining ground. They’re not a replacement for a therapist, but they help bridge the gap. One study showed a 37% drop in anxiety symptoms after 12 weeks using a digital CBT program.Which One Should You Choose?
There’s no single answer. But here’s what the latest guidelines say:- First-line? SSRIs or CBT. Both are equally recommended by the American Psychiatric Association, NICE, and the VA/DoD.
- Need fast relief? Benzodiazepines can help-but only briefly. Use them for a crisis, not for daily management.
- Depressed along with anxious? SSRIs are your best bet. They treat both.
- Want long-term results? CBT wins. You’re less likely to relapse.
- Can’t afford therapy or wait weeks for meds? Start with an SSRI. It’s more accessible than CBT and safer than benzodiazepines.

What About Combining Them?
Many people think mixing meds and therapy is the best option. And it often is. A 2022 study in JAMA Network Open found that people who got both SSRIs and CBT had a 65% remission rate-much higher than either alone. The medication helps reduce the physical symptoms enough so you can actually do the work in therapy. Therapy helps you stay off meds long-term. But it’s not always necessary. Many people do just fine with one or the other. The key is matching the treatment to your life.The Future: New Options on the Horizon
The field is changing. In 2023, the FDA approved zuranolone, a new drug that works like benzodiazepines but with far less risk of dependence. Early trials showed only 5% withdrawal symptoms, compared to 25% with traditional benzos. It’s taken as a two-week course-no daily pills, no tapering. Genetic testing is also becoming more common. Companies like GeneSight analyze your DNA to predict how you’ll respond to SSRIs. If you’re a slow metabolizer, you might get sick on standard doses. If you’re a fast one, you might need more. This isn’t mainstream yet, but it’s coming. Digital tools are expanding access. Apps, online CBT programs, and telehealth are making therapy possible for people in rural areas or with busy schedules. Insurance is slowly catching up-Medicare now covers more mental health providers than ever.What You Can Do Today
If you think you have GAD:- See your doctor. Rule out thyroid issues, vitamin deficiencies, or other medical causes.
- Ask about SSRIs. Start low. Be patient. Don’t quit if you feel worse at first.
- Look for a CBT therapist. Use Psychology Today’s directory or ask your doctor for a referral.
- If you’re already on benzodiazepines, don’t stop cold turkey. Talk to your doctor about tapering.
- Try a digital CBT app like Woebot or Sanvello. It’s not a cure, but it’s a step.
Can benzodiazepines be used long-term for GAD?
While benzodiazepines can provide fast relief, they are not recommended for long-term use in GAD. Studies show that after 3 to 6 months, most people develop tolerance, needing higher doses for the same effect. Withdrawal can be severe and even dangerous. Guidelines from NICE, the APA, and the VA/DoD all advise against using them beyond short-term crisis management. Safer, long-term options like SSRIs and CBT are preferred.
How long does it take for SSRIs to work for anxiety?
SSRIs typically take 2 to 6 weeks to show noticeable effects for anxiety. Some people may not feel improvement until week 8. This delay is normal and doesn’t mean the medication isn’t working. Side effects like nausea or jitteriness often appear first and fade within a few weeks. Starting at a low dose and increasing slowly helps reduce early discomfort.
Is CBT better than medication for anxiety?
CBT and SSRIs are equally effective in the short term. But CBT has a clear advantage in the long run. People who complete CBT are less likely to relapse after treatment ends-only 25% compared to 45% for those who stop medication. That’s because CBT teaches skills you use for life, not just while taking a pill. For lasting change, CBT is often the better choice.
Can you take SSRIs and CBT together?
Yes-and many experts recommend it. Combining SSRIs with CBT leads to higher remission rates than either treatment alone. The medication can reduce physical symptoms enough to make therapy more effective, while therapy helps prevent relapse after stopping the drug. This combination is now part of standard care in many VA clinics and integrated health systems.
What if I can’t afford therapy?
You don’t need in-person CBT to benefit. FDA-cleared digital CBT apps like Woebot, Sanvello, and SilverCloud offer structured programs based on the same principles as therapy. Studies show they reduce anxiety symptoms by 30-40% over 12 weeks. Many employers and insurers now cover these apps. Free or low-cost options are also available through community mental health centers and university clinics.

Bartholemy Tuite
November 25, 2025 AT 05:29Man, I wish I'd known all this when I was first prescribed Xanax back in '19. Thought it was magic juice. Turned into a walking zombie for 14 months. Tapering off was like getting kicked in the head every day. SSRIs took forever but at least I didn't feel like my brain was on fire when I stopped. CBT was the real game changer though - learned to stop arguing with my own thoughts. Now I just breathe and say 'nah, not today anxiety'.
Jacob McConaghy
November 25, 2025 AT 12:40Been on Lexapro for 8 months now. First 3 weeks were hell - nausea, dizziness, felt like a robot. But then one morning I woke up and realized I hadn't checked my phone for anxiety in 4 hours. That's when it clicked. SSRIs aren't a cure, they're a tool. Like putting on glasses for your brain. And yeah, sex drive took a hit, but I'd rather have peace than a raging libido.
Vineeta Puri
November 26, 2025 AT 01:49As a mental health professional in India, I must emphasize the importance of cultural context in treating GAD. While SSRIs and CBT are evidence-based, access remains a critical barrier in low-resource settings. Digital CBT platforms offer promising scalability, yet digital literacy and stigma continue to impede uptake. A holistic approach integrating community support systems alongside pharmacological and psychological interventions is essential for sustainable outcomes.
Victoria Stanley
November 26, 2025 AT 06:31Just wanted to say thank you for this post! My 16-year-old daughter was diagnosed with GAD last year. We started with Zoloft and she hated the side effects, so we switched to CBT. She's been doing online sessions twice a week for 5 months now. She says the exposure exercises feel like leveling up in a video game - scary at first but you get stronger. We're seeing real progress. No meds, just tools. It's been life-changing.
Andy Louis-Charles
November 26, 2025 AT 10:53CBT apps are legit. I tried Woebot during a rough patch at work. At first I was like 'this is dumb' but then I caught myself thinking 'wait, is that thought actually true?' and paused. That tiny moment of awareness? Priceless. Also, side note: the emoji in the app is a little turtle. 🐢 I named him Gary. He's my anxiety therapist now. No judgment.
Yvonne Franklin
November 28, 2025 AT 01:55akhilesh jha
November 28, 2025 AT 14:42Interesting how SSRIs take weeks to work but benzos work instantly. Makes me wonder if anxiety is really a chemical imbalance or just our modern life being too fast. We want instant fixes for problems that were never meant to be solved with pills. Maybe we need slower lives, not faster drugs. Just thinking out loud.
Jeff Hicken
November 28, 2025 AT 16:43SSRIs are just fancy antidepressants that make you numb. CBT? Overpriced talk therapy. Benzodiazepines? The only real solution. I've been on Xanax for 7 years and I'm fine. People who say it's addictive are just weak. Also, why do doctors always push the 'slow and steady' crap? I want relief NOW, not in 6 weeks. My boss doesn't care if I'm 'working on my brain rewiring'.
Douglas cardoza
November 30, 2025 AT 02:29My therapist told me to try CBT after 2 years of SSRIs. I was skeptical. But the first exercise? Writing down my worst fear and then listing actual evidence for/against it. I wrote 'I'll lose my job and end up homeless' and then realized I've had the same job for 12 years, saved 3 months of expenses, and my boss said I'm one of his top performers. My brain had just been lying to me. That moment changed everything.
Adam Hainsfurther
December 1, 2025 AT 15:40There's a real gap here between what the guidelines say and what actually happens in clinics. I've seen patients get benzos prescribed for 6 months because the waitlist for CBT is 11 months. Insurance won't cover more than 8 therapy sessions. And SSRIs? Doctors hand them out like candy. No follow-up, no titration. It's a system failure, not a patient failure. We need better infrastructure, not just better meds.
Rachael Gallagher
December 1, 2025 AT 15:59Big Pharma is laughing all the way to the bank. SSRIs? Designed to keep you dependent. CBT? Too expensive to scale. Benzos? Perfect for turning people into zombies who don't question the system. And now they're pushing 'zuranolone' like it's magic. Wake up. The real cure is changing society - less work, more sleep, less social media, more real connection. But that would cost too much. So we get pills.
steven patiño palacio
December 2, 2025 AT 05:04For anyone considering CBT: don't wait for perfect conditions. Start with free resources. The Centre for Clinical Interventions has excellent workbooks online. The NHS also offers free CBT modules. You don't need a $150/hour therapist to learn the basics. The principles are simple: identify the thought, challenge the evidence, reframe the narrative. Practice daily. It's like mental weightlifting. Hard at first, but your brain gets stronger.
stephanie Hill
December 2, 2025 AT 23:57Did you know SSRIs are linked to increased suicide risk in young adults? And CBT? It's just brainwashing disguised as science. The government and Big Pharma want us docile. They don't want us thinking too deeply. That's why they push these 'treatments' - to keep us quiet. My cousin went on Lexapro and became a zombie. Now she just nods and smiles at everything. That's not healing. That's suppression. The truth is out there. You just have to look beyond the brochures.