When you pick up a prescription, the label says "take with food" or "take on an empty stomach". It seems simple. But if you’ve ever forgotten which one applies to your pill, or mixed up the timing, you’re not alone. Nearly half of all prescription medications have specific food rules - and getting them wrong can mean your medicine doesn’t work, or worse, makes you sick.
Why Food Changes How Your Medicine Works
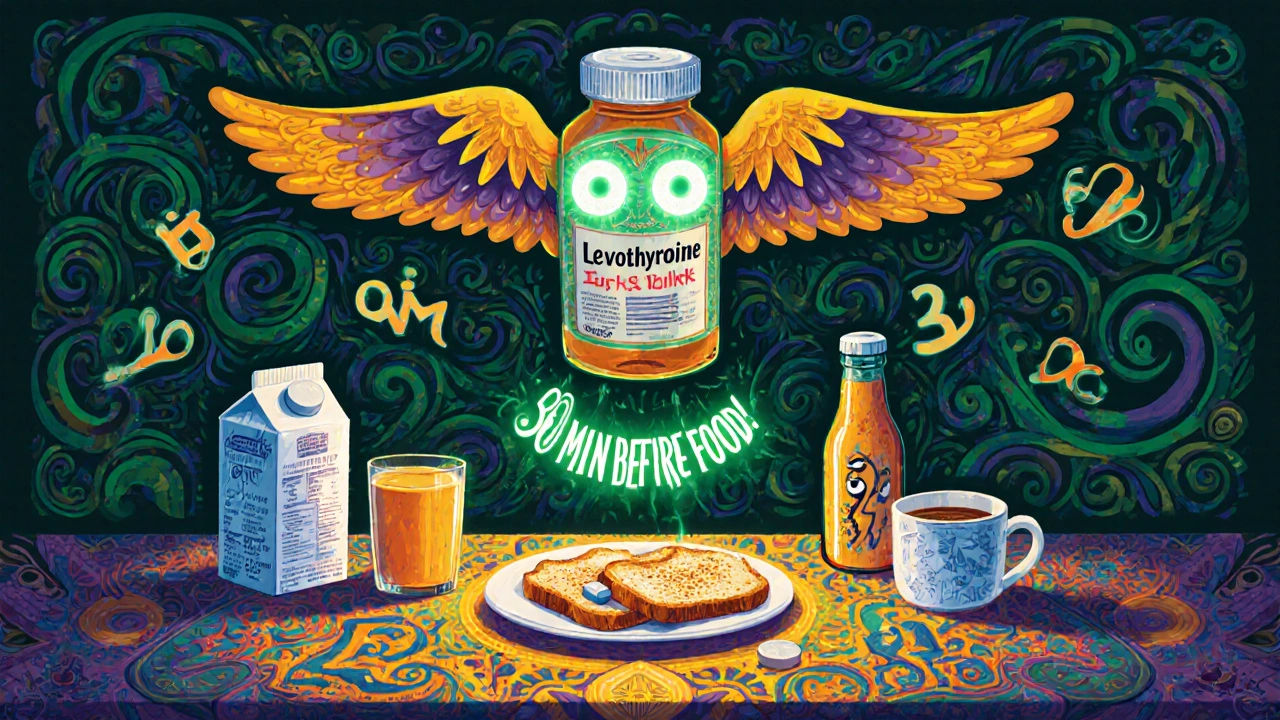
Your stomach isn’t just a place where food breaks down. It’s a chemical factory. When you eat, your body releases acid, bile, and enzymes. Blood flow changes. Your gut moves slower. All of this affects how drugs get absorbed into your bloodstream. Take a drug like levothyroxine, used for thyroid problems. If you take it with breakfast, your body might absorb 20% to 55% less of it, according to Endocrine Practice (2023). That’s not a small drop - it’s enough to leave you tired, cold, or gaining weight without knowing why. On the other hand, saquinavir, an HIV medication, absorbs up to 40% better when taken with a high-fat meal. Skip the avocado toast, and the drug might not fight the virus effectively. Food doesn’t just help some drugs work better. It can also stop others from working at all. Tetracycline and doxycycline, two common antibiotics, bind to calcium in milk, cheese, or even orange juice fortified with calcium. That binding stops the antibiotic from being absorbed. Studies show absorption can drop by up to 50%. Same goes for iron supplements and antacids - they can block absorption of other meds if taken together.Medications That Need Food
Some drugs are designed to be taken with meals. This isn’t just about comfort - it’s about safety and effectiveness. NSAIDs like ibuprofen, naproxen, and aspirin are the most common example. These can irritate your stomach lining, especially if taken on an empty stomach. The UK’s NHS and German medical guidelines both recommend taking them after eating. Why? Because food acts like a buffer. It reduces the chance of ulcers, bleeding, or severe heartburn. One 2021 study in the Journal of Antimicrobial Chemotherapy found that taking Augmentin (amoxicillin/clavulanate) with food cut nausea by 20%. That’s huge for people who already feel sick. Antiretrovirals like ritonavir and zidovudine (AZT) also need food. Taking them on an empty stomach often leads to nausea and vomiting. Reddit users on r/HIV reported that taking ritonavir with a small high-fat snack - like peanut butter or cheese - dropped nausea from 45% to just 18%. That’s not luck. It’s science. Fat helps slow digestion, letting the drug absorb more steadily. Nitrofurantoin (Macrobid) and rifabutin (Mycobutin) are other antibiotics that are easier on the stomach when taken with food. The NHS England says food can extend their effective window from 20-60 minutes to up to two hours, meaning fewer doses are needed to keep the drug level steady.Medications That Must Be Taken on an Empty Stomach
Not all drugs like food. Some actually get destroyed or blocked by it. Levothyroxine is the classic example. It needs to be taken 30 to 60 minutes before breakfast. Even a cup of coffee or a piece of toast can interfere. A 2024 Mayo Clinic guide says the timing matters more than you think - if you take it with food, your thyroid levels might never stabilize, no matter how consistent your dose. Didanosine, an older HIV drug, is broken down by stomach acid. Food increases acid production, which destroys the drug before it can be absorbed. That’s why it’s strictly an empty-stomach med. Tetracycline and doxycycline are also on this list. As mentioned, calcium, magnesium, aluminum, and iron - all found in dairy, antacids, or multivitamins - bind to these antibiotics and prevent absorption. Even a glass of milk can ruin an entire dose. Bisphosphonates like alendronate (Fosamax), used for osteoporosis, require even stricter rules. You must take them first thing in the morning with a full glass of water, then wait 30 to 60 minutes before eating, drinking, or lying down. If you don’t, the drug can irritate your esophagus or not absorb at all.
What About Grapefruit Juice?
Grapefruit juice isn’t just a breakfast staple - it’s a hidden drug interaction risk. It blocks an enzyme in your gut called CYP3A4, which normally breaks down certain medications. When that enzyme is blocked, the drug builds up in your blood - sometimes to dangerous levels. This affects drugs like saquinavir, some statins (like simvastatin), and certain blood pressure meds. One study in Clinical Infectious Diseases (2019) showed grapefruit juice boosted saquinavir levels even more than a high-fat meal. That’s why many doctors now say: if your med says "avoid grapefruit," they mean it. No exceptions.Why People Get It Wrong - And How to Fix It
A 2023 GoodRx survey found that 42% of people who take five or more medications have accidentally taken one the wrong way - with food when they shouldn’t, or without food when they should. It’s not laziness. It’s complexity. You might have five pills. One needs food. One needs an empty stomach. One can’t be near dairy. One needs to be taken at bedtime. One requires a full glass of water. It’s easy to mix them up. The solution? Systems. Pharmacists at Express Scripts created a color-coded label system: red for "empty stomach," green for "with food," and yellow for "with high-fat meal." In a six-month pilot, this boosted adherence by 31%. Simple. Visual. Effective. Smartphone reminders also help. Reddit users on r/Pharmacy reported a 68% success rate when they set alarms for medication times. One user set three alarms: one for 7 a.m. (empty stomach med), one for 8 a.m. (with breakfast), and one for 8 p.m. (with dinner). They said it turned chaos into routine. But the biggest factor? Understanding why. The American Pharmacists Association found that patients who knew why their medicine had food rules were 44% more likely to follow them. If you know that taking your antibiotic with milk means it won’t work, you’re more likely to leave the yogurt behind.
What to Do Right Now
Don’t guess. Don’t assume. Here’s what to do today:- Look at every prescription label. If it says "take with food" or "take on empty stomach," write it down.
- Ask your pharmacist: "Is there a specific time I should take this? Should I avoid anything like dairy, grapefruit, or coffee?"
- Use a pill organizer with labeled sections for morning, afternoon, and night.
- Set phone alarms for each dose - not just the time, but the rule: "7 a.m. - empty stomach, water only."
- If you’re taking more than three meds, ask for a medication review. Many pharmacies offer this free.
Matthew Mahar
November 24, 2025 AT 04:14Okay but like… I took my doxycycline with a yogurt parfait once and thought I was being healthy?? 😅 My stomach still hates me. Now I just chug it with water and run away from dairy like it’s a horror movie. Why does food have to be so complicated??
Richard Wöhrl
November 26, 2025 AT 00:03Really appreciate this breakdown. The levothyroxine point is critical-many patients don’t realize even coffee can interfere. I’ve seen patients take it with their morning espresso and wonder why TSH stays elevated. The 30-60 min window isn’t arbitrary; it’s pharmacokinetics. Also, the grapefruit warning needs to be screamed from rooftops. I’ve had patients on simvastatin who thought "a little juice" was fine. Spoiler: it’s not.
And yes, color-coded labels? Genius. My pharmacy started doing that last year. Adherence jumped. People aren’t lazy-they’re overwhelmed. Give them visual cues, not jargon.
Also: the FDA’s new labeling rules? Long overdue. "Take with food" is meaningless. Is it a salad? A steak? A donut? Be specific. Science deserves precision.
Kezia Katherine Lewis
November 26, 2025 AT 14:03The CYP3A4 inhibition by grapefruit is one of the most underappreciated pharmacokinetic phenomena in clinical practice. The furanocoumarins irreversibly inhibit intestinal CYP3A4, leading to prolonged elevation of plasma concentrations-sometimes for up to 72 hours after ingestion. This isn’t a "don’t drink it" suggestion; it’s a potentially lethal interaction profile for statins, calcium channel blockers, and certain immunosuppressants. The WHO’s inclusion of food-specific instructions on the Essential Medicines List reflects a global recognition of bioavailability as a public health equity issue-not just a pharmacology footnote.
shreyas yashas
November 26, 2025 AT 17:41Bro, I’m from India and we take all our medicines with chai. Turns out, our turmeric lattes and milk tea are wrecking our antibiotics. I had to stop taking doxycycline with breakfast after my skin infection came back. Now I drink chai after my meds. Small change, big difference.
Kane Ren
November 28, 2025 AT 13:02This is the kind of post that saves lives. Seriously. I used to mix up my meds until I started using a pill box with alarms. Now I feel like a boss. You’re not just taking pills-you’re running your body like a well-oiled machine. Keep it up!
John Mackaill
November 29, 2025 AT 13:46I’ve been on ritonavir for 8 years. The peanut butter trick? Lifesaver. I used to puke every morning. Now I eat a spoonful with my pill-no nausea, no stress. It’s not magic. It’s bioavailability. But most docs don’t explain it. They just say "take with food." Thank you for spelling out why.
Dalton Adams
December 1, 2025 AT 09:33Let’s be real: if you can’t remember whether to take your pill with or without food, you probably shouldn’t be managing your own meds. This isn’t a "tips for forgetful people" article-it’s a warning sign. You need a caregiver. Or at least a pharmacist on speed dial. The fact that 42% of polypharmacy patients mess this up is a systemic failure. Not a personal one.
Also, AI predicting gut bacteria interactions? That’s not the future. It’s already here. And if you’re still using "take with food" labels in 2025, you’re part of the problem.
Suresh Ramaiyan
December 1, 2025 AT 11:37It’s funny how we treat medicine like it’s just a thing you swallow. But it’s alive in your body. It reacts to what you eat, when you eat, even what you drink. Food isn’t just fuel-it’s a co-pilot. Sometimes it helps. Sometimes it sabotages. Understanding that shift-from passive consumer to active participant-is the real medicine.
Adrian Rios
December 3, 2025 AT 07:22I’ve been a pharmacy tech for 14 years and I still see people taking levothyroxine with their multivitamin at breakfast. Same with bisphosphonates-people take them with orange juice because "it’s healthy," then complain about esophageal pain. The science is clear, but the communication? Broken. We need more than labels-we need stories. We need to tell patients: "This isn’t about rules. It’s about your thyroid working. It’s about your infection clearing. It’s about not ending up in the ER because you thought grapefruit was harmless." The difference between compliance and understanding? That’s the gap we need to bridge. And honestly? If you’re taking more than three meds, you deserve a medication coach. Not just a pharmacist handing you a bottle.
Also, the color-coded system? That’s not innovation-that’s basic human-centered design. Why didn’t we do this 20 years ago?
And yes, the FDA’s update? Finally. But now we need to train every prescriber, every pharmacist, every nurse to use the new language. No more "with food." No more "avoid dairy." We need: "Take 60 minutes before eating anything, including coffee. Do not consume calcium, iron, or magnesium within 4 hours."
And if you’re on simvastatin? Don’t even look at a grapefruit. Not even in a photo. Not even in a juice commercial. I’m not joking. I’ve seen the numbers. It’s not worth the risk.
Charmaine Barcelon
December 4, 2025 AT 19:29Ugh. So much overthinking. Just take your pills when you remember. If you feel bad, stop. Simple. Why do we need color codes and alarms and AI? People used to live longer before all this tech nonsense.
Casper van Hoof
December 6, 2025 AT 00:54The ontological implications of pharmaceutical bioavailability, when contextualized within the phenomenology of daily routine, reveal a profound dissonance between medical prescription and lived embodiment. The alimentary canal, far from being a passive conduit, functions as an active epistemic site where pharmacological intentionality is either realized or subverted by the contingent variables of dietary ingestion. One is thus compelled to ask: Is adherence an act of compliance-or a surrender to the hegemony of clinical temporality?
Brandy Walley
December 7, 2025 AT 15:14Y’all are making this way too hard. My grandma took every pill with a beer and lived to 92. If it works, it works. Stop scaring people.
Matthew Mahar
December 8, 2025 AT 10:32Wait… so if I take my doxy with peanut butter, am I basically doing the same thing as the HIV folks? 🤯