Ever wonder why some pills are called lisinopril, others Prinivil, and a third group has a name like 1-[(2-ethyl-1H-imidazol-5-yl)methyl]-2-methyl-5-nitro-1H-imidazole? It’s not random. There’s a whole system behind how drugs get their names - and it’s designed to save lives.
Why Drug Names Matter More Than You Think
Medication errors kill over 250,000 people in the U.S. every year. That’s more than car accidents or breast cancer. A big part of that? Confusing drug names.
Imagine a nurse grabbing a bottle labeled Hydralazine but grabbing Hydroxyzine by accident. One treats high blood pressure. The other is for allergies. Mix them up? Bad outcomes. That’s why drug names aren’t chosen by marketing teams alone - they’re built with science, safety, and global clarity in mind.
There are three layers to every drug’s identity: chemical, generic, and brand. Each has a job. Understand them, and you’ll never look at a prescription the same way again.
Chemical Names: The Molecular Blueprint
If you opened up a drug molecule under a microscope, you’d see atoms - carbon, oxygen, nitrogen - arranged in a precise structure. The chemical name is the full scientific description of that structure, written using rules from the International Union of Pure and Applied Chemistry (IUPAC).
Take propranolol. Its chemical name? 1-(Isopropylamino)-3-(1-naphthyloxy)propan-2-ol. That’s 42 characters. No one says that at the pharmacy. But it’s essential for scientists. It tells you exactly how the molecule is built - where the oxygen sits, how the rings connect, what side chains are attached.
Chemical names are like DNA sequences for drugs. They’re precise, unambiguous, and universal. But they’re useless in clinics. Too long. Too hard to spell. Too easy to misread. That’s why we have generic names.
Generic Names: The Safety Code
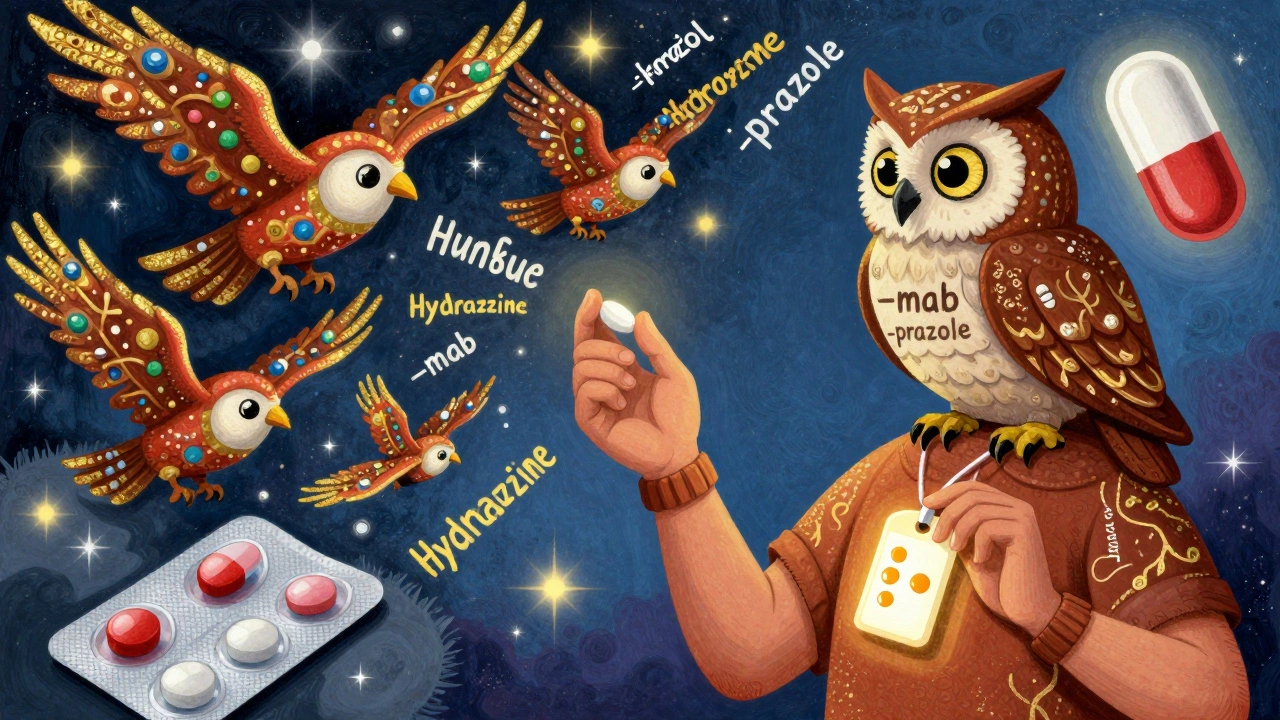
Generic names - also called nonproprietary names - are the workhorses of safe prescribing. They’re assigned by international bodies like the World Health Organization (WHO) and the U.S. Adopted Names (USAN) Council. These names follow strict patterns that tell you what the drug does before you even look it up.
Here’s how it works: Stems tell you the class. Prefices make each drug unique.
- Drugs ending in -prazole? Proton pump inhibitors - used for acid reflux. Omeprazole, esomeprazole, pantoprazole.
- End in -tinib? Tyrosine kinase inhibitors - cancer drugs. Imatinib, sunitinib, erlotinib.
- End in -mab? Monoclonal antibodies. Adalimumab, rituximab, trastuzumab.
- End in -citinib? Janus kinase inhibitors. Tofacitinib, upadacitinib.
These stems aren’t random. They’re standardized across 150+ countries. A doctor in Tokyo, a pharmacist in Lagos, and a nurse in Chicago all recognize -prazole as a stomach acid reducer. That’s global safety.
The USAN Council reviews over 300 proposed generic names a year. About 30% get rejected. Why? Because they sound too similar to existing drugs. Fluoxetine and Fluphenazine were nearly rejected because of the “-xine” ending. Too close. Too dangerous.
Dr. Robert M. Goggin, former head of the USAN Council, says standardized stems reduce medication errors by 27%. That’s not a guess. That’s data from real hospital error logs.

Brand Names: The Marketing Layer
Now you see the same drug sold under different names. Lisinopril is the generic. Prinivil and Zestril are brand names. Same pill. Same active ingredient. Different packaging, different price.
Pharmaceutical companies spend millions developing brand names. They want something catchy, easy to remember, and trademarkable. But they can’t just pick anything.
The FDA has a team that reviews every brand name proposal. They check for:
- Similarity to existing drug names (sound, spelling, appearance)
- Unintended meanings in other languages
- Therapeutic claims (no “HeartHeal” or “PainStop”)
- Confusion with over-the-counter meds or supplements
One in three brand name submissions get rejected. In 2022, a company tried to name a new antidepressant Deprex. The FDA blocked it - too close to Depakote, a seizure drug. Another wanted Cardiva. Too similar to Cardizem, a blood pressure med. Both were denied.
Brand names also have to include the generic name on every ad. You’ll see “Lisinopril (Prinivil)” in commercials. That’s not just for transparency - it’s a legal requirement.
Company Codes: The Internal ID
Before a drug even hits a lab, it has a code. Pfizer uses “PF-” followed by numbers. Merck uses “MK-”. Roche uses “RO-”.
For example, the drug now called abrocitinib was once Pfizer PF-04965842-01. The first part is the company. The numbers are the compound ID. The last two digits? The salt form.
These codes aren’t meant for patients. They’re for scientists tracking the molecule through clinical trials. One compound might have 50 different internal codes as it’s tested in different doses, forms, or combinations.
It’s like a birth name before you get your official name. The company code is the drug’s original identity - before it’s given a name the world can use.
Why Generic and Brand Drugs Look Different
You might notice that generic versions of your pill look different. Smaller. Different color. Odd shape. That’s not a mistake.
U.S. law says generic drugs must have the same active ingredient, strength, dosage form, and route as the brand. But they don’t have to look the same. Why? Trademark law.
If a generic looked exactly like the brand, it could confuse patients - and legally, it might be seen as copying the brand’s identity. So generics are made to look different. That’s why your blue oval pill becomes a white oval, or a pink capsule.
But here’s the catch: 347 medication errors in 2022 were linked to confusion over pill appearance. Patients thought their new pill was the wrong drug. Pharmacists had to double-check.
That’s why knowing the generic name matters more than the color or shape.
What’s Changing Now?
Drug names aren’t frozen in time. New types of medicines need new naming rules.
RNA-based therapies? New stem: -siran. Peptide-drug conjugates? -dutide. Targeted protein degraders? Coming soon: -tecan.
Since 2021, the USAN Council uses AI to screen names. It scans 15,000 existing drug names in milliseconds, checking for phonetic and visual similarities. It cut confusion risks by 42% in its first year.
And the WHO now assigns about 200 new generic names every year. Since 1953, over 10,000 have been created. That’s a living system - constantly adapting to new science.
What Patients Should Know
Most patients don’t know the difference between generic and brand names. A 2022 FDA survey found 68% of patients felt confused by generic names - especially long ones like secukinumab or ixekizumab.
But pharmacists? 83% say standardized naming makes their job safer. They can spot a potential mix-up faster because of the stems.
Here’s what you can do:
- Always ask: “What’s the generic name?” Write it down.
- If your pill looks different, check the label - it’s probably the generic version.
- Don’t assume a brand is better. Generics are just as effective - same active ingredient, same FDA approval.
- If a name sounds familiar, double-check. Hydralazine vs. Hydroxyzine - one letter changes everything.
Drug names aren’t just labels. They’re safety tools. Every syllable, every stem, every letter was chosen to prevent harm.
What’s Next?
As drugs get more complex - gene therapies, cell therapies, AI-designed molecules - naming will get even more critical. The system we have now was built for pills and injections. Now we’re dealing with living cells and RNA snippets.
But the goal hasn’t changed: make sure the right drug gets to the right patient, every time. No guesswork. No confusion. Just clarity.
Next time you pick up a prescription, look at the name. Not just the brand. Look at the generic. See the stem. That’s not just a name - it’s a lifesaving code.
What’s the difference between a generic name and a brand name?
The generic name is the official scientific name for the active ingredient in a drug, assigned by regulatory agencies like the WHO or USAN Council. It’s the same across all brands. The brand name is created by the pharmaceutical company for marketing and is protected by trademark. For example, the generic name is ibuprofen; brand names include Advil and Motrin. Both contain the same active ingredient, but only the brand name can be advertised as a product.
Why do generic drugs look different from brand-name drugs?
By law, generic drugs must have the same active ingredient, strength, and effectiveness as the brand. But they don’t have to look the same. Trademark rules prevent generics from copying the exact color, shape, or size of the brand name version. This avoids confusion and protects the brand’s intellectual property. Differences in appearance don’t affect how the drug works.
Are generic drugs as safe and effective as brand-name drugs?
Yes. The FDA requires generics to meet the same strict standards as brand-name drugs. They must contain the same active ingredient, in the same amount, and work the same way in the body. Differences in inactive ingredients (like fillers or dyes) don’t change effectiveness. Over 90% of prescriptions filled in the U.S. are generics - and they’re used safely every day in hospitals and clinics worldwide.
How are drug names chosen?
Drug names go through a multi-step process. First, the company assigns an internal code. Then, during clinical trials, a generic name is proposed using standardized stems (like -prazole or -mab) to show the drug’s class. The USAN or WHO reviews it for safety and clarity - rejecting about 30% for sounding too similar to existing names. Brand names are submitted later to the FDA, which checks for confusion, language issues, and false claims. The whole process takes 4-7 years.
What do the endings like -prazole or -mab mean?
Those are stems - standardized suffixes that tell you the drug’s class and how it works. For example, drugs ending in -prazole (like omeprazole) reduce stomach acid. Those ending in -mab (like adalimumab) are monoclonal antibodies used in autoimmune and cancer treatments. Stems help doctors and pharmacists quickly identify what a drug does, even if they’ve never heard the name before. This reduces errors and improves safety.
Can drug names cause medication errors?
Yes. Similar-sounding or similarly spelled names are a leading cause of medication errors. For example, Hydralazine (for high blood pressure) and Hydroxyzine (for allergies) sound alike - and have led to dangerous mix-ups. The FDA and WHO reject names that are too close to existing ones. Still, errors happen. That’s why knowing the generic name and recognizing stems is critical for safety.
Do other countries use the same drug names?
Yes - for generic names. The WHO’s International Nonproprietary Names (INN) program ensures that a drug called metformin in the U.S. is called metformin in India, Brazil, or Germany. This global standardization helps prevent errors when drugs are shipped or prescribed across borders. Brand names, however, can vary by country - so a drug might be sold as Glucophage in the U.S. and Glucophage or another name elsewhere, but the generic stays the same.
Drug nomenclature isn’t just jargon - it’s a silent guardian in every pharmacy, hospital, and clinic. When you understand how names work, you’re not just reading a label. You’re reading a safety protocol.

Aidan Stacey
December 10, 2025 AT 18:05Bro this is wild. I never realized that -mab or -prazole actually tell you what the drug does. I thought they were just fancy sci-fi words. Now I look at my blood pressure med and go ‘ohhh that’s a calcium channel blocker’ like I’m some kind of medical wizard. 🤓
Courtney Blake
December 11, 2025 AT 18:32Typical American overcomplication. We spend billions naming drugs so no one dies from a typo, but our hospitals still can’t figure out how to print legible prescriptions. Meanwhile, China just calls everything by the molecule and moves on. We’re not safe-we’re performative.
Sylvia Frenzel
December 12, 2025 AT 19:41Ugh. Another article pretending drug naming is some noble science. It’s corporate branding with a lab coat. The FDA ‘rejects’ names? Please. They just delay the inevitable so the pharma company can spend another $2M on lawyers. Wake up.
Paul Dixon
December 13, 2025 AT 06:00Love this breakdown. I used to panic when my pills changed color-thought I got the wrong stuff. Now I just check the generic name. Life’s so much simpler when you know the code. Thanks for making this feel less like a textbook 😊
john damon
December 14, 2025 AT 07:20OMG I JUST REALIZED MY ANTIBIOTIC IS A -MYCIN 😱 I’M LITERALLY TAKING A DRUG WITH A STEM THAT SAYS ‘ANTIBIOTIC’ IN IT. THIS IS THE BEST THING I’VE LEARNED SINCE I FOUND OUT ‘TETRACYCLINE’ MEANS ‘FOUR RINGS’ 🤯🧪
Monica Evan
December 14, 2025 AT 18:05So many people think generics are cheap knockoffs but they’re literally the same molecule. I work in a rural clinic-we use generics because brand names cost 10x and people skip doses because they can’t afford it. The stem system? It’s the only thing keeping us from giving someone allergy meds for heart failure. No joke. This system saves lives daily
Jean Claude de La Ronde
December 16, 2025 AT 17:21Ah yes, the noble art of naming things so precisely that no one can pronounce them. We give molecules 42-character names and then wonder why patients forget their meds. Meanwhile, in Quebec, we just call it ‘the blue pill for high blood’ and everyone’s happy. Progress is overrated.
Jim Irish
December 17, 2025 AT 21:14Standardized nomenclature reduces errors. Data confirms this. Generic names are not marketing tools. They are clinical safety instruments. Brand names are secondary. This is not opinion. This is regulatory science.
Mia Kingsley
December 18, 2025 AT 10:49Wait so you’re telling me the FDA rejected ‘Deprex’ because it sounded like ‘Depakote’ but let through ‘Zoloft’? Zoloft sounds like a robot sneezing. And ‘Lexapro’? That’s not a drug, that’s a spaceship. Who approved this? 😅
Katherine Liu-Bevan
December 20, 2025 AT 06:23One of the most underappreciated systems in modern medicine. The stem-based naming convention is brilliant-international, scalable, and designed for safety, not profit. It’s why a nurse in Nairobi can safely dispense metformin without knowing English. That’s engineering with humanity in mind.
Lisa Stringfellow
December 21, 2025 AT 21:23Yeah sure, ‘it saves lives’-but how many people died because some intern misspelled ‘-tinib’ as ‘-tineb’ and the AI didn’t catch it? This whole system is just a glorified game of telephone with a billion-dollar budget.
Kristi Pope
December 22, 2025 AT 07:52This is honestly one of the coolest things I’ve read all year. I used to think drug names were just made up by marketers with too much caffeine. Now I see them as this quiet, genius language built by scientists to keep us alive. I’m gonna start saying ‘-mab’ like it’s a secret handshake 🫶