Have you ever started a new medication and suddenly felt sick-even though you were taking a sugar pill? Or switched to a generic version of your drug and started experiencing side effects you never had before? If so, you might not be reacting to the medicine. You might be reacting to your expectations.
What Exactly Is the Nocebo Effect?
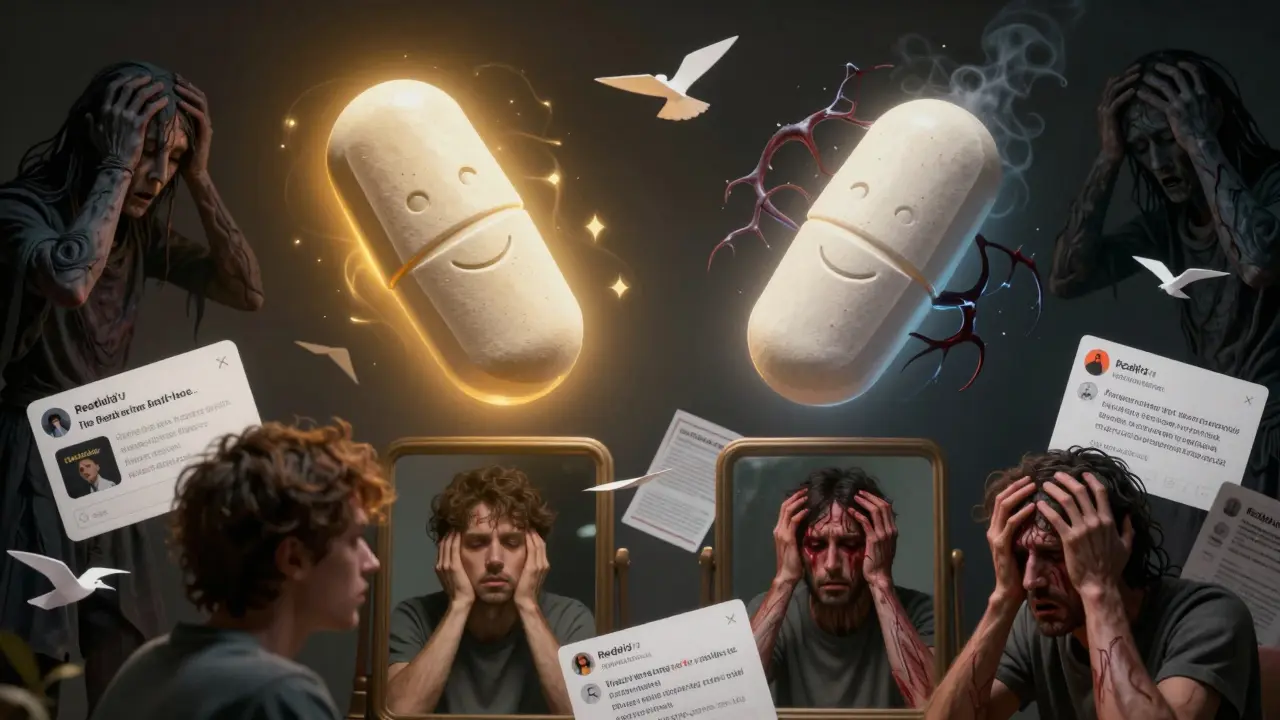
The nocebo effect is the dark twin of the placebo effect. While the placebo effect happens when you feel better because you believe a treatment will work-even if it’s just a sugar pill-the nocebo effect is when you feel worse because you believe something bad is going to happen. The word comes from Latin: nocebo means "I will harm." It’s not magic. It’s biology.
When you’re told a drug might cause nausea, dizziness, or fatigue, your brain starts scanning your body for those symptoms. A normal ache? That’s the medication. A little tired after work? Must be the pills. Your brain doesn’t wait for chemicals to act-it triggers real physical changes just from what you expect. Brain scans show that negative expectations light up the same areas as real pain: the anterior cingulate cortex, the insula, and the prefrontal regions. These are the same spots that fire when you stub your toe or get a headache.
Here’s the kicker: in clinical trials, about 20% of people taking a placebo report side effects. Nearly 10% quit the trial because they felt so bad. And yet, they weren’t taking any active drug. Their bodies were responding to words, tone, and fear-not chemistry.
Real-Life Examples: When the Pill Isn’t the Problem
In 2017, New Zealand switched millions of patients from brand-name venlafaxine to a cheaper generic version. The active ingredient? Exactly the same. But after media coverage warned people about "potential differences" in side effects, reports of nausea, dizziness, and anxiety jumped dramatically. The number of adverse event reports to the national monitoring system rose by over 40%-even though the drug hadn’t changed.
On Reddit, users post stories like: "I switched from brand-name sertraline to generic and got terrible insomnia. My pharmacist said it might be psychological. I went back to the brand, and the symptoms vanished." The active ingredient didn’t change. The packaging did. The expectation did. And that was enough to trigger real symptoms.
Studies show that the more side effects listed on a medication leaflet, the more people report them. One study found that patients who received leaflets with 15 side effects listed were twice as likely to report those symptoms than those who got leaflets with only five-even when both groups got identical pills.
How the Nocebo Effect Works in Your Brain
It’s not just "in your head." It’s in your nervous system, your hormones, your pain pathways. When you expect harm, your body releases stress chemicals like cortisol and adrenaline. These can tighten muscles, raise your heart rate, make you nauseous, or even lower your pain threshold.
Think of it like this: your brain is constantly predicting what your body should feel. If you’ve been told a drug causes headaches, your brain starts interpreting any mild head pressure as a headache-even if it’s just from dehydration or stress. This is called symptom amplification. Your brain doesn’t ignore normal sensations anymore. It amplifies them.
There’s also misattribution. You had a headache yesterday. You start the new pill today. Now your brain links the two-even if the headache had nothing to do with the medication. And then there’s heightened awareness. Suddenly, you’re hyper-focused on every twinge, every burp, every yawn. Is that fatigue? Is that dizziness? Or just life?
One landmark study gave people a powerful painkiller, remifentanil. When they were told it would relieve pain, it worked. When they were told it might make their pain worse after the effect wore off? The painkiller stopped working entirely. Just by changing the words, researchers erased the drug’s effect. No extra dosage. No chemical change. Just expectation.
Who’s Most at Risk?
Not everyone experiences the nocebo effect the same way. Some people are more vulnerable:
- Women: In placebo-controlled trials, women report side effects 23% more often than men. Why? It’s not biology alone-it’s how they’re warned. Studies suggest women are more likely to receive detailed side effect warnings.
- People with anxiety or depression: They’re 1.7 times more likely to experience nocebo effects. Their brains are already wired to scan for threats.
- Pessimistic thinkers: If you tend to expect the worst, your brain is primed to notice and amplify negative signals.
- Those influenced by media or social stories: A viral post, a news headline, or even a friend’s horror story can trigger a cascade of symptoms.
It’s not about being "weak-minded." It’s about how your brain processes information. The nocebo effect isn’t a flaw-it’s a survival mechanism gone overboard.
Why This Matters for Your Health
The nocebo effect isn’t just a curiosity. It’s costing lives and money.
Between 15% and 20% of patients stop taking effective medications because they believe they’re causing side effects. That means people are going off blood pressure drugs, antidepressants, or cholesterol meds-not because the drugs failed, but because they thought they did. This leads to worse health outcomes: uncontrolled diabetes, heart attacks, depression relapses.
Pharmaceutical companies lose billions each year because patients switch away from effective generic drugs after hearing scary stories. The global generic drug market is worth over $200 billion. And yet, only 32% of major drug companies train their patient education teams to avoid triggering nocebo responses.
Healthcare systems are starting to notice. The UK’s NHS cut medication-related adverse event reports by 14% in pilot areas just by changing how doctors talk about side effects. New Zealand’s healthcare system reduced discontinuation rates by 20% after training providers to frame risks differently.

How to Fight the Nocebo Effect
You can’t ignore risks. But you can communicate them better.
Here’s what works:
- Don’t lead with the worst. Instead of saying, "This drug can cause severe nausea in 15% of users," say, "Most people feel fine. A small number may feel a bit queasy, but it usually passes in a few days."
- Normalize normal symptoms. "It’s common to feel a little tired when starting this. That doesn’t mean it’s not working-it means your body is adjusting."
- Ask about expectations. "Have you heard anything about this medication before?" That opens the door to correct myths before they take root.
- Use neutral language. Avoid phrases like "dangerous side effects" or "rare but serious." Say "possible effects" or "what some people notice."
- Give context. "This side effect happens in 1 out of 10 people. But 9 out of 10 feel better overall."
Patients who get this kind of communication are less likely to quit their meds. They’re also more likely to stick with treatment long-term-even if they feel a little off at first.
The Bigger Picture: Expectations Shape Reality
The nocebo effect proves something powerful: your mind doesn’t just react to the world. It helps build it. What you expect, your body prepares for. What you fear, your body manifests.
This isn’t about dismissing real side effects. Some drugs do cause real harm. But a huge chunk of what we call "side effects" isn’t from the pill-it’s from the story we’ve been told about the pill.
As research continues, we’re learning that even telling someone they’re taking a placebo can still help them feel better-if you frame it right. Open-label placebos, where patients know they’re taking a sugar pill but are told it can still work through mind-body connections, are showing promise in chronic pain and IBS studies.
The future of medicine isn’t just better drugs. It’s better conversations.
What You Can Do
If you’re starting a new medication:
- Ask your doctor: "What do most people feel when they start this?"
- Don’t read the leaflet the moment you get it. Wait until you’ve talked to your provider.
- Notice if you’re looking for symptoms. Are you checking your body every hour? That’s a sign your brain is primed for the nocebo effect.
- Give it time. Most side effects fade in a week or two. If they don’t, talk to your doctor-but don’t assume it’s the drug.
If you’re a caregiver or healthcare provider:
- Use positive framing. Focus on what most people experience, not the rare worst-case.
- Ask open questions. "What are you worried about?" is more helpful than "Do you have any concerns?"
- Don’t overload. One or two key risks matter more than a list of 20.
Can the nocebo effect cause real physical damage?
Yes, but not in the way most people think. The nocebo effect doesn’t damage organs or cause disease. But it can trigger real physiological changes-like increased stress hormones, higher blood pressure, muscle tension, or altered pain perception. These can make symptoms feel severe enough to stop treatment, which then leads to real health risks from untreated conditions. So while the effect itself isn’t toxic, the consequences of believing in it can be.
Is the nocebo effect the same as hypochondria?
No. Hypochondria (now called illness anxiety disorder) is a mental health condition where someone fears they have a serious illness despite medical reassurance. The nocebo effect is different: it’s triggered by specific expectations about a treatment, not general health anxiety. Someone with nocebo symptoms might feel sick after taking a pill, but they don’t necessarily think they have cancer. They think the pill made them sick. It’s context-specific and tied directly to medical experiences.
Can you get nocebo effects from online reviews?
Absolutely. Studies show that reading negative reviews of medications increases the likelihood of reporting side effects-even if you’ve never taken the drug. Online forums, YouTube videos, and social media posts create vivid mental images of harm. When you later take the drug, your brain uses those images as a template. That’s why stories like "I got dizzy after switching to generic" spread so fast-they’re not just anecdotes. They’re nocebo triggers.
Why do generic drugs cause more side effect reports than brand-name ones?
They’re chemically identical-but psychologically different. Brand-name drugs come with years of trust, marketing, and familiarity. Generics are often seen as "inferior," even when they’re not. Media coverage, pharmacist warnings, and patient stories all feed into the belief that generics are riskier. In New Zealand, when a brand-name drug switched to generic, adverse event reports spiked-not because the drug changed, but because people expected it to.
Can doctors prevent the nocebo effect?
Yes, by changing how they communicate. Training programs in Europe and New Zealand show that doctors who learn to frame side effects positively reduce patient discontinuation rates by up to 20%. Simple phrases like "Most people feel fine," "This usually passes quickly," or "This is your body adjusting" make a huge difference. It’s not about hiding risks-it’s about balancing them with context and reassurance.

Nina Catherine
February 19, 2026 AT 15:58