Prasugrel Benefit-Risk Calculator
This tool estimates the potential benefits and bleeding risks of prasugrel based on patient factors. Remember: prasugrel is not recommended for patients with a history of stroke or TIA due to increased bleeding risk.
Key Takeaways
- Prasugrel is a third‑generation P2Y12 inhibitor that reduces clot formation after a heart attack or stent placement.
- Large trials (TRITON‑TIMI 38) show prasugrel cuts the risk of repeat heart attacks by about 20% compared with clopidogrel, but it raises bleeding risk.
- It is not the first choice for patients with a history of stroke or transient ischemic attack because of higher intracranial bleeding rates.
- Dosage is simple-60mg loading dose then 10mg daily, with adjustments for weight <60kg or age≥75years.
- Regular monitoring, especially for signs of bleeding, is essential when using prasugrel as part of dual antiplatelet therapy.
Every year, millions of people experience a stroke or a heart attack caused by a clot that forms in a narrowed artery. Doctors rely on antiplatelet medicines to keep platelets from sticking together, but not all drugs work the same way. When the conversation turns to newer, more potent options, prasugrel often pops up. Below you’ll discover what the drug does, why it matters for preventing clot‑related events, and the trade‑offs you should weigh before starting it.
What Is Prasugrel?
Prasugrel is a prescription antiplatelet classified as a third‑generation P2Y12‑receptor inhibitor. It belongs to the thienopyridine family, a group that also includes clopidogrel and ticlopidine. By binding irreversibly to the platelet P2Y12 receptor, prasugrel blocks ADP‑induced activation, a key step in platelet aggregation.
Unlike older thienopyridines, prasugrel is converted to its active metabolite more efficiently by hepatic enzymes, giving it a faster and more consistent onset of action.
How Prasugrel Works to Reduce Stroke and Heart Attack Risk
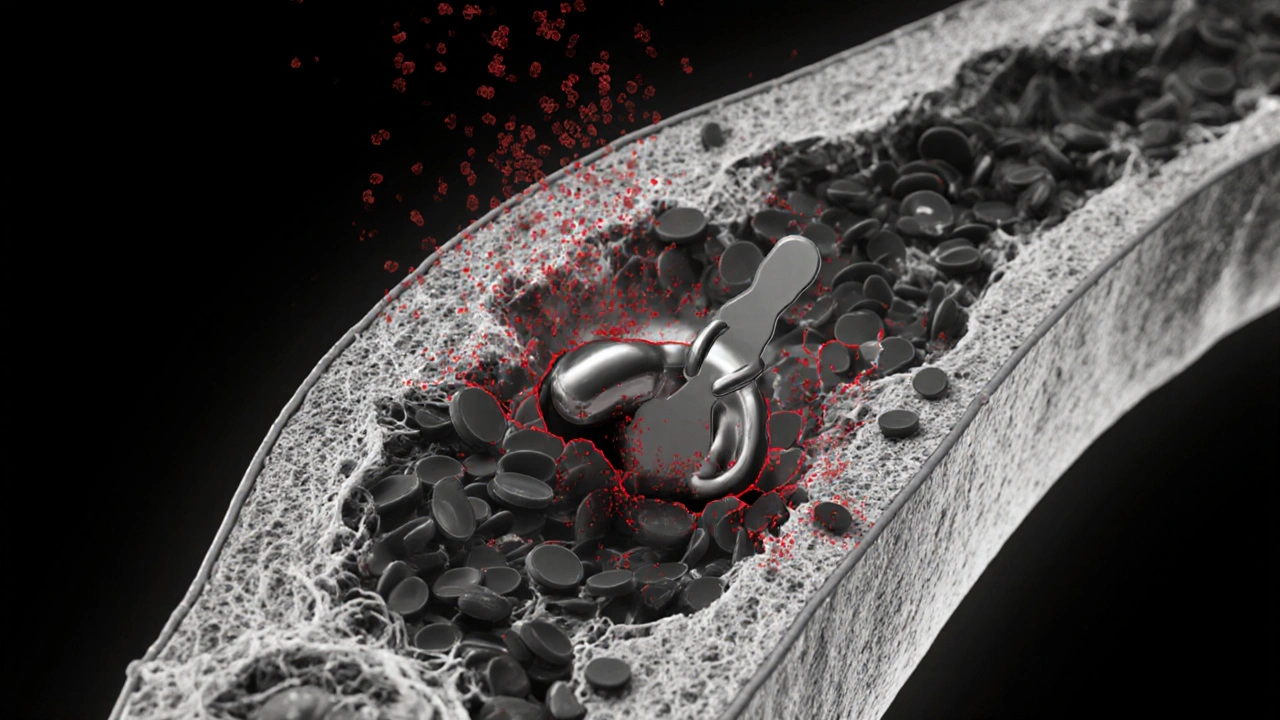
The cascade that leads to a clot starts when a ruptured plaque exposes collagen and tissue factor. Platelets rush to the site, release ADP, and bind to the P2Y12 receptor on neighboring platelets. This binding amplifies aggregation and stabilises the clot.
By blocking the P2Y12 receptor, prasugrel cuts off the ADP signal, preventing the platelet “crowd” from forming. The result is fewer occlusive clots in coronary arteries (reducing heart attacks) and in cerebral arteries (reducing ischemic strokes).
Prasugrel is usually prescribed as part of dual antiplatelet therapy (DAPT), paired with low‑dose aspirin. The combination targets two different pathways: aspirin blocks thromboxaneA2, while prasugrel blocks ADP.

Clinical Evidence Supporting Prasugrel
The biggest proof comes from the TRITON‑TIMI 38 trial, which enrolled more than 13,000 patients with acute coronary syndrome (ACS) who received a coronary stent. Participants were randomized to receive either prasugrel (60mg loading, then 10mg daily) or clopidogrel (600mg loading, then 75mg daily).
- Primary endpoint (cardiovascular death, myocardial infarction, or stroke) occured in 9.9% of the prasugrel group versus 12.1% of the clopidogrel group (hazard ratio0.81).
- Stent thrombosis dropped from 2.3% to 1.4%.
- Major bleeding (including intracranial) rose from 1.4% to 2.0%.
Sub‑analyses showed that patients without a prior stroke or transient ischemic attack (TIA) derived the greatest net benefit. For those with a history of stroke/TIA, the bleeding risk outweighed the modest reduction in ischemic events, leading to a FDA‑issued contraindication for that subgroup.
Other studies, such as the CERTITUDE registry (real‑world data from Europe), confirmed comparable effectiveness but highlighted that clinicians often reduce the maintenance dose to 5mg for patients <60kg or >75years to tame bleeding.
Comparing Prasugrel with Other Antiplatelet Drugs
| Attribute | Prasugrel | Clopidogrel | Ticagrelor |
|---|---|---|---|
| Onset of action | 30‑60min | 2‑6hrs | 30‑60min |
| Reversibility | Irreversible | Irreversible | Reversible |
| Major trial | TRITON‑TIMI 38 | CLARITY‑TIMI 28 | PLATO |
| Relative reduction in MI | ~20% vs clopidogrel | Reference | ~15% vs clopidogrel |
| Major bleeding ↑ | 1.8‑2.0% (vs 1.4% clopidogrel) | 1.4% | 1.6% (vs 1.4% clopidogrel) |
| Contraindicated in prior stroke/TIA | Yes | No | No |
In plain language, prasugrel is more potent than clopidogrel and a bit more consistent than ticagrelor, but you pay a higher price in bleeding risk. Ticagrelor’s reversible binding makes it attractive for patients who might need surgery soon, while aspirin remains the backbone of DAPT.
Safety, Side Effects, and Who Should Avoid It
Bleeding is the headline adverse effect. Because prasugrel blocks platelet function for the lifespan of the platelet (7‑10days), any bleed can be harder to control.
- Common: bruising, nosebleeds, gastrointestinal upset.
- Serious: intracranial hemorrhage, life‑threatening gastrointestinal bleed.
Risk factors that amplify bleeding include:
- Age≥75years
- Body weight <60kg
- History of prior stroke or TIA (contraindicated)
- Concomitant anticoagulants (warfarin, DOACs)
Patients with severe liver disease or active pathological bleeding should also avoid prasugrel. If a patient develops a major bleed, the drug’s effect can only be offset by platelet transfusion or, in rare cases, by using a P2Y12‑reversal agent under investigation (e.g., bentracimab).

Practical Guidance: Dosage and Monitoring
The standard regimen for a typical adult undergoing percutaneous coronary intervention (PCI) is a 60mg loading dose followed by 10mg daily. Adjustments are recommended as follows:
- Weight <60kg → 5mg daily
- Age≥75years → 5mg daily (even if weight >60kg)
Patients should continue the drug for at least 12months after a drug‑eluting stent (DES), unless bleeding forces an early stop. Regular follow‑up includes:
- Baseline CBC and periodic hemoglobin checks.
- Assessment for signs of occult GI bleed (dark stools, fatigue).
- Review of any over‑the‑counter NSAID use.
Because prasugrel is metabolised by CYP2C19 and CYP3A4, strong inhibitors (e.g., ketoconazole) can raise active metabolite levels and further increase bleeding risk.
Bottom Line
If you’ve had an ACS event and a stent was placed, prasugrel offers a powerful way to keep arteries clear. It shines in patients under 75years, weighing more than 60kg, and without prior stroke/TIA. The trade‑off is a modestly higher bleeding chance, so doctors must balance the benefits against each patient’s bleed profile.
Always discuss with your cardiologist whether the drug fits your personal risk picture, and never stop or change the dose without medical guidance.
Frequently Asked Questions
What makes prasugrel different from clopidogrel?
Prasugrel is converted to its active form more reliably and works faster, giving a stronger, more predictable inhibition of platelet aggregation. This translates into a lower rate of repeat heart attacks but also a higher bleeding risk.
Can prasugrel be used after a stroke?
No. The FDA and EMA label prasugrel as contraindicated in anyone who has had an ischemic stroke or a transient ischemic attack because the drug raises the chance of intracranial bleeding in that group.
How long should I stay on prasugrel after a stent?
Guidelines recommend at least 12months of dual antiplatelet therapy after a drug‑eluting stent. Some clinicians shorten the course if bleeding becomes a problem, but any change should be discussed with a cardiologist.
What are the signs of a serious bleed while on prasugrel?
Watch for sudden severe headache, visual changes, slurred speech (possible brain bleed), vomiting blood, black/tarry stools, or a rapid drop in blood pressure. Any of these symptoms require immediate medical attention.
Is there an antidote for prasugrel?
Currently, no specific reversal agent is approved. Management focuses on supportive care and platelet transfusion. Research is ongoing into agents like bentracimab that could neutralise P2Y12 inhibitors.
Justin Channell
October 16, 2025 AT 17:46Prasugrel can be a game changer 💪
Basu Dev
October 18, 2025 AT 11:26The TRITON‑TIMI 38 trial, which enrolled over 13,000 patients with acute coronary syndrome, demonstrated that prasugrel reduced the composite endpoint of cardiovascular death, myocardial infarction, or stroke when compared with clopidogrel, showing a relative risk reduction of roughly 20 percent. This benefit was especially pronounced in patients who received a coronary stent, as the more potent platelet inhibition helped prevent stent thrombosis. The study also highlighted that prasugrel’s faster onset of action and more consistent inhibition of the P2Y12 receptor contributed to its efficacy. However, the same trial reported a higher incidence of major bleeding events, including intracranial hemorrhage, particularly among patients with a prior history of stroke or transient ischemic attack. The dosing regimen consists of a 60 mg loading dose followed by a maintenance dose of 10 mg daily, which may be reduced to 5 mg in patients weighing less than 60 kg or older than 75 years. In clinical practice, the decision to use prasugrel often balances the reduced risk of ischemic events against the increased bleeding risk, guided by patient-specific factors such as age, weight, and comorbidities. Current guidelines recommend prasugrel as a reasonable alternative to clopidogrel in patients undergoing percutaneous coronary intervention who are not at high risk for bleeding. For patients with a known history of stroke, however, clopidogrel or ticagrelor may be preferred due to the safety profile. Moreover, drug–drug interactions are minimal, but caution is advised when co‑administering with other anticoagulants. The pharmacokinetic profile of prasugrel shows rapid absorption and conversion to its active metabolite, achieving peak platelet inhibition within hours. Long‑term adherence is essential, as premature discontinuation can negate the protective benefits against recurrent myocardial infarction. Real‑world data corroborate the trial findings, indicating that appropriate patient selection maximizes the net clinical benefit. While the cost of prasugrel may be higher than generic clopidogrel, the reduction in repeat revascularization procedures can offset expenses in certain healthcare settings. Ongoing research continues to explore the role of prasugrel in diverse populations, including those with diabetes or chronic kidney disease. Ultimately, the clinician’s judgment, informed by a thorough risk‑benefit assessment, determines the optimal antiplatelet strategy for each individual patient.
Krysta Howard
October 18, 2025 AT 14:13While the data are impressive, we can’t ignore the serious bleeding concerns – especially intracranial bleeds – that make prasugrel a risky choice for many patients 😬. The trial numbers are solid, but in everyday practice the trade‑off often tips toward safety first.
nica torres
October 19, 2025 AT 23:33Wow, looks like prasugrel could really boost protection after a heart attack! 🌟 Just remember to keep an eye on those bleed warnings.
Dean Marrinan
October 20, 2025 AT 01:46Oh sure, because what we really need is another “miracle drug” that comes with a side‑effect checklist the size of a grocery list 😂. At least the emojis are on point.
Oluseyi Anani
October 21, 2025 AT 13:53Guidelines clearly state that prasugrel should be avoided in anyone with a prior stroke due to the heightened intracranial bleeding risk – an essential point for clinicians to remember.
Rahul yadav
October 21, 2025 AT 16:23It’s heartbreaking to think a life‑saving drug can turn dangerous in the very brain that needs protection 😢. The balance between clot prevention and hemorrhage is a delicate dance.
Jonny Arruda
October 22, 2025 AT 22:56Prasugrel’s stronger platelet inhibition is great for stent patients, but the bleeding risk is a real concern.
Ryan Pitt
October 23, 2025 AT 00:53Exactly, especially for those with low body weight or older age – dose adjustment is key.
Jami Johnson
October 24, 2025 AT 08:50The increased potency of prasugrel undeniably cuts down repeat myocardial infarctions, yet the literature also flags a surge in major bleeding events, particularly intracranial hemorrhage, making patient selection paramount. Physicians must weigh the benefit of reduced ischemic events against the potentially catastrophic consequences of bleeding, especially in patients with prior cerebrovascular incidents. Moreover, the drug’s dosing flexibility-adjusting to 5 mg for those under 60 kg or over 75 years-offers a mitigative strategy, but vigilance remains essential.
Ryan Moodley
October 24, 2025 AT 10:30Ah, the classic “benefit‑risk” debate-always a convenient excuse to avoid taking a firm stance. If you’re so worried about bleeding, maybe just stick with the old drug and call it a day.
carol messum
October 25, 2025 AT 19:50Interesting read-makes you think about how we balance efficacy and safety.
Jennifer Ramos
October 25, 2025 AT 21:13Indeed, the article is clear, but note the slight typo in the dosage section: it should be “adjustments for weight, age, and renal function,” not just “weight”.
Grover Walters
October 27, 2025 AT 06:56From a pharmacological perspective, prasugrel’s irreversible platelet inhibition raises the stakes for any subsequent surgical procedures, necessitating careful peri‑operative planning.
Amy Collins
October 27, 2025 AT 08:03Cool info, but honestly the bleeding risk is a deal‑breaker for most patients.
amanda luize
October 28, 2025 AT 20:10One must wonder if pharmaceutical big‑shots are quietly steering guidelines toward drugs like prasugrel to inflate their bottom line, all while downplaying the ominous specter of intracranial hemorrhage. The narrative seems engineered for profit, not patient safety.
Chris Morgan
October 28, 2025 AT 21:00While conspiracy theories abound the data remain clear no meta‑analysis has shown a net mortality benefit over clopidogrel