Adrenal incidentaloma is a mass in the adrenal gland found accidentally during imaging for another reason. It’s not caused by symptoms and usually discovered during CT or MRI scans. About 2% of adults have these masses, but the chance goes up with age-over 7% in people over 70. While most are harmless, some can cause serious health issues. Here’s how doctors decide what to do.
Why evaluation is necessary
Even though adrenal incidentalomas often cause no symptoms, they can hide serious problems. Some produce excess hormones, leading to issues like high blood pressure or diabetes. Others might be cancerous. Skipping evaluation could mean missing a treatable condition or having unnecessary surgery. For example, a pheochromocytoma (a rare tumor) can cause life-threatening blood pressure spikes during surgery if not detected first.
How doctors evaluate adrenal incidentalomas
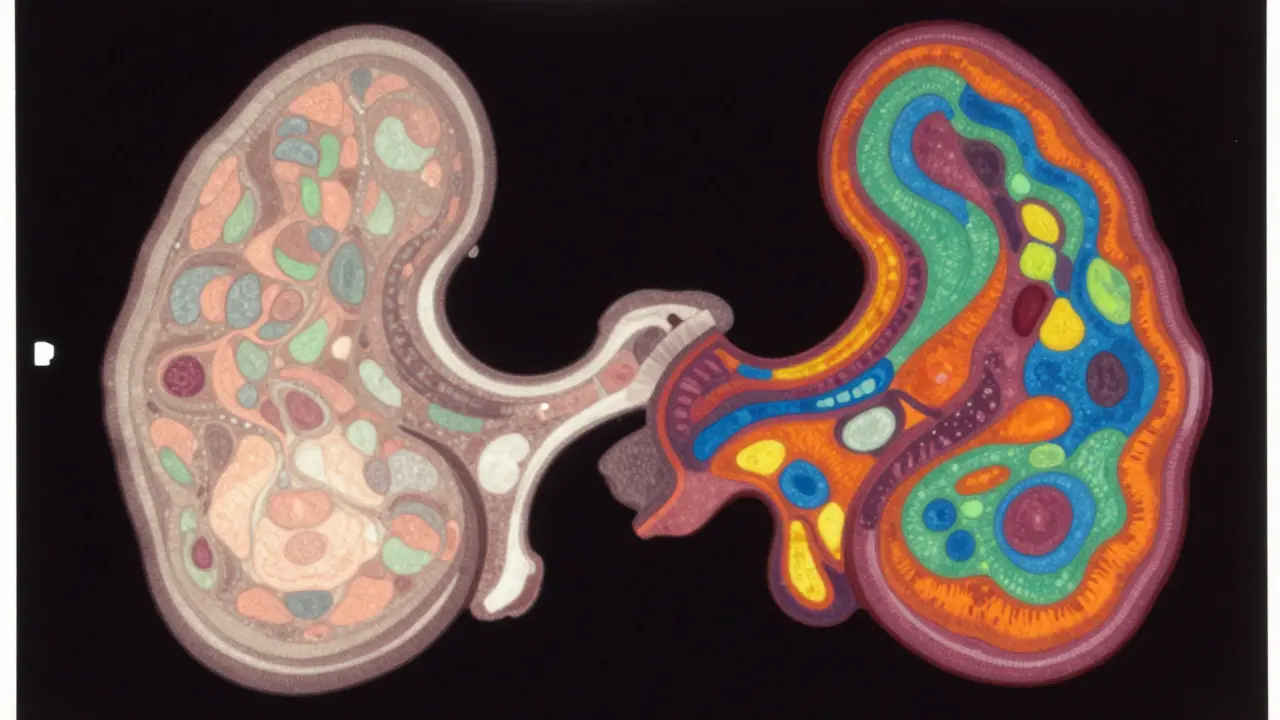
Evaluation starts with imaging and hormone tests. The first step is usually a CT scan without contrast. This helps check the mass’s size and density. A CT scan shows Hounsfield units (HU), a measure of density. If the mass has less than 10 HU, it’s likely a benign adrenal adenoma. But if it’s higher, more tests are needed.
| Feature | Benign Adenoma | Suspicious for Malignancy |
|---|---|---|
| Attenuation (HU) | < 10 | > 10 |
| Enhancement | Homogeneous | Heterogeneous |
| Shape | Smooth, round | Irregular, lobulated |
| Growth rate | Stable or slow | Rapid (>1 cm/year) |
Testing for hormone overproduction
Doctors check for three main hormone issues. First, pheochromocytoma: a tumor that makes adrenaline-like hormones. They test plasma-free metanephrines or 24-hour urine metanephrines. High levels mean surgery is needed to avoid dangerous blood pressure spikes during surgery. Second, cortisol excess: tested with a 1 mg dexamethasone suppression test. If cortisol stays above 1.8 μg/dL after the test, it suggests subclinical Cushing’s syndrome. Third, aldosterone excess: checked in people with high blood pressure or low potassium. They measure plasma aldosterone and renin levels. If aldosterone is high and renin low, it could be primary hyperaldosteronism.

When surgery is needed
Surgery is recommended for several reasons. Any tumor larger than 4 cm has a higher cancer risk. All hormone-producing tumors need removal, regardless of size. Also, if imaging shows signs of cancer-like irregular shape, fast growth, or high density-surgery is necessary. For pheochromocytoma, doctors give alpha-blockers for 1-2 weeks before surgery to prevent blood pressure crises. Adrenocortical cancer, though rare, requires surgery if possible. But if the tumor is small, non-functional, and shows no cancer signs, no treatment is needed. Just keep an eye on it with yearly scans.
After surgery: recovery and monitoring
Most adrenal surgeries are done laparoscopically, which means small cuts and faster recovery. Patients usually go home in 1-2 days. After removing a hormone-producing tumor, symptoms often improve quickly. For example, blood pressure normalizes in many with aldosterone issues. However, if the whole adrenal gland is removed, patients might need lifelong hormone replacement. Follow-up care includes regular check-ups to ensure no recurrence, especially for cancer cases.
Can an adrenal incidentaloma go away on its own?
No, adrenal incidentalomas don’t disappear without treatment. However, many are harmless and don’t require any action. They’re typically monitored with imaging to ensure they don’t grow or change. Only about 20% need intervention, so most people can live normally without surgery.
What are the risks of not treating a functional adrenal tumor?
Untreated hormone-producing tumors can cause serious health problems. A pheochromocytoma may trigger life-threatening blood pressure spikes during stress or surgery. Cortisol excess can lead to diabetes, osteoporosis, or heart disease. Aldosterone excess causes high blood pressure and kidney damage. Early treatment prevents these complications.
Is adrenal surgery dangerous?
Adrenal surgery is generally safe when done by experienced teams. Laparoscopic procedures have low complication rates (under 5%) and quick recovery. However, skipping preoperative preparation for pheochromocytoma can cause dangerous blood pressure spikes during surgery. Always work with a specialist team to minimize risks.
What happens if a tumor is cancerous?
Adrenocortical carcinoma (ACC) is rare but aggressive. Surgery is the main treatment if the tumor is localized. Chemotherapy or radiation may follow. Early detection improves outcomes-5-year survival is 60-80% for small tumors but drops to 20-40% if it spreads. Regular follow-up is critical for recurrence monitoring.
How often should I get follow-up scans?
For benign non-functioning tumors under 4 cm with no cancer signs, yearly CT scans are usually enough. If the tumor is indeterminate (unclear if benign), scans every 6-12 months for 2 years are recommended. Hormone-producing tumors need immediate surgery, so follow-up focuses on recovery and symptom management.
