What Is CRPS, and Why Does It Hurt So Much?
Complex Regional Pain Syndrome, or CRPS, isn’t just a bad ache that won’t go away. It’s a nervous system glitch - a misfire where pain signals keep screaming even after the original injury has healed. Imagine stubbing your toe, and weeks later, your foot still burns like it’s on fire, even when you brush against a sock. That’s CRPS. It often starts after a fracture, surgery, or sprain, but the pain doesn’t match the damage. In fact, the pain gets worse over time, spreading beyond the injury site. Your skin might change color, swell up, or feel freezing cold or burning hot. And the worst part? Even light touch can feel like needles.
Doctors used to call it Reflex Sympathetic Dystrophy, but now we know it’s not about the sympathetic nerves alone. It’s about your brain. Years of research show that CRPS rewires how your brain maps your body. The area that represents your painful hand or foot gets blurry, mixed up with neighboring areas. This is called cortical smudging. Your brain stops recognizing your limb as normal. So when you move it, or someone touches it, your brain interprets it as danger - even when there’s no real threat.
Why Traditional Therapy Often Fails
Many patients start with physical therapy - stretching, strengthening, range-of-motion exercises. But if your brain is screaming danger every time you move, those exercises can make things worse. Pushing through pain doesn’t retrain the brain. It just teaches it that movement equals more pain. Studies show that traditional therapy alone reduces pain by only about 1.5 points on a 10-point scale after 12 weeks. That’s barely noticeable. And for many, the frustration leads to quitting.
CRPS isn’t a muscle problem. It’s a brain problem. You can’t stretch your way out of a misfiring nervous system. That’s why newer, neuroscience-based approaches like desensitization and graded motor imagery have become the gold standard. They don’t try to force the body to move. They fix the brain’s misunderstanding of the body.
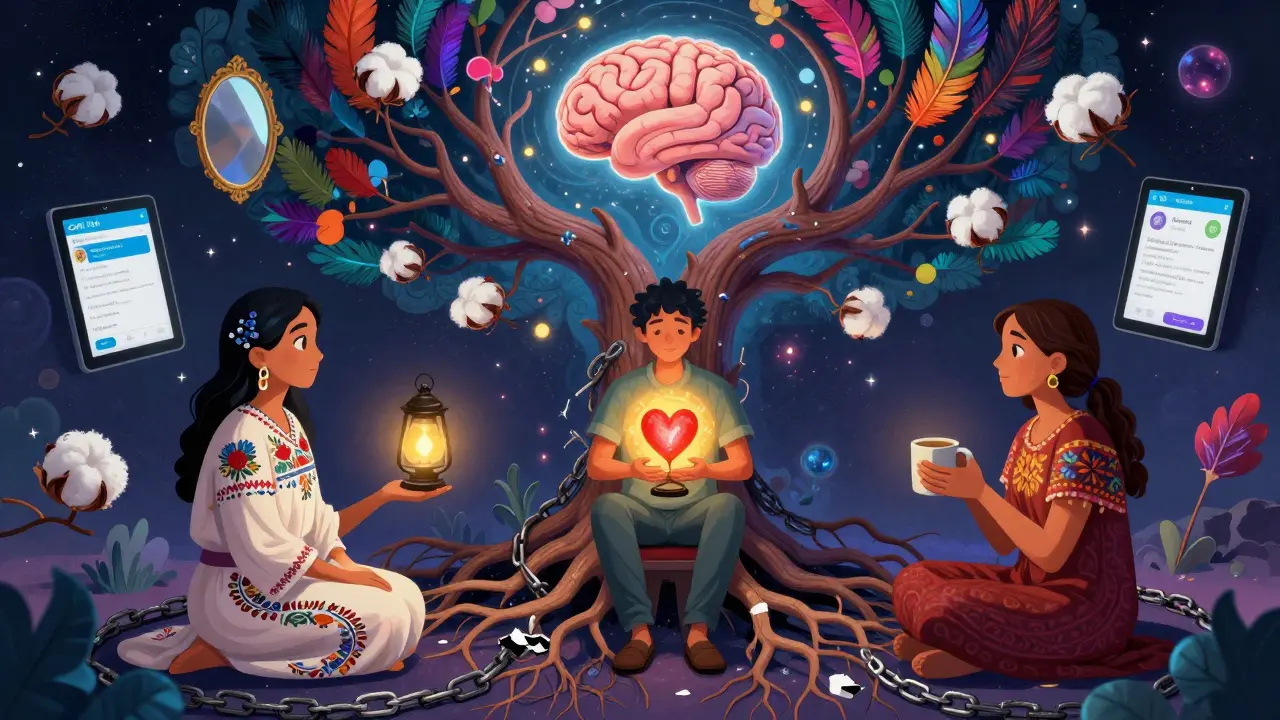
Desensitization: Rewiring Your Skin’s Alarm System
One of the most painful symptoms of CRPS is allodynia - where something that shouldn’t hurt, like a breeze or fabric, feels like fire. Desensitization therapy teaches your brain that these sensations aren’t dangerous. It’s not about toughening up your skin. It’s about rewiring your nervous system.
The process starts slow. Really slow. You begin with something as light as a cotton ball, brushing it over your skin for just 5 minutes at a time, three to five times a day. The pressure? Less than 10 grams - about the weight of a paperclip. You don’t push through pain. You stop if your pain goes above 3 out of 10. Progress isn’t measured in weeks, but in tolerance. Once you can handle the cotton ball without pain spiking, you move to silk. Then to a soft towel. Then to denim. Eventually, you work up to wearing regular clothes again.
A 2021 study with 127 patients showed those who did structured desensitization improved 42% more on hand function tests than those who didn’t. Why? Because fMRI scans revealed a 30-40% drop in brain activity in the area that processes touch. Your brain stops overreacting. It learns that touch isn’t a threat.
Therapists break this into four phases: passive touch with eyes open, then active movement during touch, then adding temperature (cooling or warming), and finally, full functional use. It takes 4 to 12 weeks. It’s boring. It’s frustrating. But it works.

Graded Motor Imagery: Training Your Brain to Move Again
Graded Motor Imagery (GMI) is the most powerful tool we have for CRPS. It was developed by Dr. G. Lorimer Moseley and his team in Australia in the early 2000s. Unlike physical therapy, GMI doesn’t move your limb at all - at first. It starts in your mind.
GMI has three stages. First: left-right discrimination. You look at pictures of hands or feet - some left, some right - and you click which one you see. Sounds simple? Try it with your own CRPS-affected limb. Most people get it wrong half the time. That’s because your brain’s map of that limb is scrambled. You’re not just guessing - your brain doesn’t know what it’s looking at anymore.
You do 50 images a day. You aim for 90% accuracy, with each answer under 1.5 seconds. Apps like Recognise Online help track your progress. When you hit that target, you move to stage two: motor imagery. You close your eyes and imagine moving your painful hand - like picking up a cup - but you don’t move it. You just think about it. For 5 to 10 minutes a day. No pain. No strain. Just mental rehearsal.
Stage three is mirror therapy. You put your good hand in front of a mirror, and your painful hand behind it, hidden. When you move your good hand, the mirror makes it look like your painful hand is moving normally. Your brain sees movement without pain. It starts to believe the limb is safe again.
In a 2006 study, 70% of CRPS patients had a 50% drop in pain after just four weeks of GMI. Brain scans showed the blurred area in their somatosensory cortex returned to normal size. That’s not luck. That’s neuroplasticity - your brain healing itself.
Why Combining Both Works Better
Desensitization and GMI aren’t competitors. They’re teammates. Desensitization calms the alarm system in your skin and spinal cord. GMI fixes the broken map in your brain. Together, they attack CRPS from both ends.
A 2022 review of 33 studies found that GMI reduced pain by 2.8 points more than traditional therapy. But when you add desensitization and cognitive behavioral therapy, the pain drop jumps to 5.2 points over 24 weeks. That’s the difference between living in constant discomfort and getting back to daily life.
Patients who stick with both report life-changing results. One Reddit user said after three months of GMI, their hand temperature went from 82°F to 96°F - normal. Another said they could finally wear socks again after 18 months. These aren’t outliers. They’re the norm when the protocol is followed correctly.
What Can Go Wrong - And How to Avoid It
These therapies are powerful, but they’re not magic. And they’re not DIY. If you rush them, you can make things worse.
Most failures happen because people move too fast. Jumping from cotton to sandpaper in a week? Your brain will shut down. Advancing GMI before hitting 90% accuracy? You’ll reinforce pain. A 2022 audit found 35% of treatment failures were due to speeding up the process. Another 22% failed because no psychological support was included - and CRPS is as much emotional as it is physical.
Therapists need special training. The American Physical Therapy Association says only therapists with at least 40 hours of CRPS-specific training should run GMI. Look for Certified Hand Therapists (CHT) or those trained by the NOI Group. If your therapist doesn’t know what left-right discrimination is, walk out.
And don’t expect quick wins. The first two weeks of GMI often make pain worse. One YouTube creator said her pain spiked 30% at first. But by week six, she could pick up a coffee cup. That’s the pattern. It gets harder before it gets easier.
Who Benefits the Most - And Who Might Not
CRPS rehabilitation works best when started early. The Cleveland Clinic found 83% success rates when treatment began within three months. After a year? Only 42%. Time matters. The longer your brain holds onto the pain map, the harder it is to rewrite.
But not everyone can do GMI. People with severe cognitive issues - like dementia or an MMSE score under 24 - struggle with the mental tasks. Those with major vision problems can’t use mirror therapy or digital apps. And if you’re too overwhelmed by anxiety or depression, the mental focus needed for motor imagery may be too much.
That’s why multidisciplinary care is key. A pain psychologist, occupational therapist, and physical therapist working together gives you the best shot. It’s not just about moving your hand. It’s about healing your whole nervous system.
Where to Find Help - And What’s New
Access to these therapies is still uneven. In the U.S., 78% of big medical centers offer GMI, but only 42% of rural clinics do. That’s a gap. But telehealth is closing it. A 2022 study showed 67% of remote patients still benefited from virtual GMI sessions.
New tech is helping too. Apps like Miro Therapeutics, cleared by the FDA in 2022, guide you through GMI with AI. They track your progress, adjust difficulty, and remind you to stay consistent. One study found 35% higher adherence than traditional methods.
And the NHS in England now requires GMI to be offered within four weeks of referral. That’s policy changing because the science is solid. The International Association for the Study of Pain has made CRPS rehabilitation a top research priority, funding $15 million a year through 2030.
What to Do Next
If you have CRPS, don’t wait. Start by asking your doctor for a referral to a certified hand therapist or pain specialist trained in GMI and desensitization. Don’t settle for generic PT. Ask if they use the NOI Group protocol. Bring a printed copy of the Budapest Criteria - it’s the official diagnostic standard.
Track your pain daily. Use a 10-point scale. Note what triggers it. Write down your progress, even if it’s slow. Celebrate small wins - like wearing a glove, or holding a warm mug without flinching.
And remember: CRPS is not your fault. It’s not weakness. It’s a neurological condition. And the science now gives you real tools to take it back. You don’t need to live in pain. Your brain can heal. You just need the right path.
Alex Smith
January 10, 2026 AT 23:19Also, 90% accuracy on left-right discrimination before moving to motor imagery? That’s not therapy, that’s a video game level. And I’m here for it.
Priya Patel
January 12, 2026 AT 22:26Michael Patterson
January 14, 2026 AT 06:54Also, ‘cortical smudging’? That’s not a real term. You just made that up to sound smart.
Priscilla Kraft
January 15, 2026 AT 22:58Week 2: pain spiked. Week 4: I cried because I held a coffee cup without screaming. Week 12: I hugged my niece. I didn’t flinch.
This isn’t placebo. It’s neuroplasticity. And if you’re still doubting, just ask someone who’s lived it.
Vincent Clarizio
January 15, 2026 AT 23:39Desensitization isn’t ‘rubbing cotton on your skin.’ It’s neural re-education. You’re not conditioning your skin - you’re reprogramming your limbic system. The somatosensory cortex isn’t just ‘blurred’ - it’s been erased by fear, and GMI is the CTRL+Z of neurology.
And don’t even get me started on how the pharmaceutical industry hates this because it doesn’t involve pills. No profit in rewiring a brain, right? Only in selling opioids until the patient ODs. I’ve seen it. I’ve lived it. And I’m not shutting up until every doctor in America knows what GMI stands for.
Also, the fact that the NHS now mandates it? That’s the kind of policy change that should make you cry. Not from sadness - from relief. We’re finally moving from ‘treat the symptom’ to ‘heal the system.’ And it’s beautiful.
Christian Basel
January 16, 2026 AT 05:30Also, ‘cortical smudging’? That’s not a neuroanatomical term. It’s a metaphor. And metaphors don’t belong in clinical literature. You’re conflating poetic language with scientific rigor. This reads like a blog post written by a grad student who just read Moseley’s TED Talk.
Matthew Miller
January 17, 2026 AT 21:34You’re selling hope like it’s a supplement. And you know what? People will buy it. Because they’re desperate. But that doesn’t make it valid. Where’s the longitudinal data? Where’s the peer-reviewed replication? You cite one 2006 study and act like it’s gospel. Pathetic.
Alfred Schmidt
January 18, 2026 AT 05:45But here’s the thing - when you finally, FINALLY, pick up your coffee cup without your whole body seizing up - you don’t celebrate. You just sit there. Because you realize: you’ve been living in a cage your whole life, and you didn’t even know the door was unlocked.
And now? I can hug my kid. I can hold my wife’s hand. I can wear a shirt without feeling like I’m being stabbed.
This isn’t ‘therapy.’ This is resurrection. And if you’re still skeptical? Go sit with someone who’s been through it. Not a doctor. Not a study. A real person. Then come back and tell me it’s all in their head.
Roshan Joy
January 19, 2026 AT 02:50Madhav Malhotra
January 19, 2026 AT 12:44But I’m sending this to every physio I know. Maybe one day, we’ll have this too. Until then - thank you for not giving up on us.
Sam Davies
January 19, 2026 AT 14:02Meanwhile, in the real world, people are still being told their pain is ‘psychogenic’ because their MRI came back ‘normal.’ You’re not fixing the system. You’re just giving the suffering a new brand.
Jennifer Littler
January 19, 2026 AT 23:50Also - yes, the first two weeks suck. You’ll feel worse. That’s not failure. That’s neuroplasticity fighting back. Like rehabbing a sprained ankle - you don’t heal by avoiding pain. You heal by safely re-exposing the system.
Do the work. Find a CHT. Don’t let the cynics derail you. This isn’t woo. It’s neuroscience with heart.